About Hyperparathyroidism
Definition
Hyperparathyroidism occurs when too much parathyroid hormone is released by the parathyroid glands in the neck. It generally leads to high levels of calcium in the blood. Endocrine glands secrete hormones necessary for the normal functioning of the body.
Our body has four parathyroid glands. They are small, pea-sized glands, located in your neck just behind our butterfly-shaped thyroid gland. Two parathyroid glands lie behind each ‘wing’ of your thyroid gland. Parathyroid hormone has a number of effects in our body:
- It causes bone to release calcium.
- It causes calcium to be taken up into our blood (absorbed) from our gut (small intestine).
- It stops our kidneys from getting rid of (excreting) calcium in our urine.
- It causes our kidneys to excrete phosphate in our urine.
In Hyperparathyroidism, our parathyroid glands make and release too much parathyroid hormone. Generally, this means that the calcium level in our blood becomes too high.
Most people with primary disease have no symptoms at the time of diagnosis. In those with symptoms the most common is kidney stones with other potential symptoms including weakness, depression, bone pains, confusion, and increased urination. Both types increase the risk of weak bones.
Causes and Types of Hyperparathyroidism
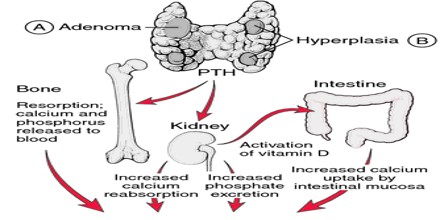
In Hyperparathyroidism, one or more of our parathyroid glands becomes overactive and makes excess PTH. This could be due to a tumor, gland enlargement, or other structural problems of the parathyroid glands. When our calcium levels are too low, our parathyroid glands respond by increasing the production of PTH. This causes our kidneys and intestines to absorb a larger amount of calcium. It also removes more calcium from our bones. PTH production returns to normal when our calcium level goes up again.
There are three types of hyperparathyroidism: primary, secondary, and tertiary.
Primary Hyperparathyroidism – In primary hyperparathyroidism, one or more of our parathyroid glands become enlarged and overactive. The gland, or glands, releases too much parathyroid hormone. This results in a high level of calcium in our blood.
Causes include:
- A single parathyroid adenoma.
- Hyperplasia affecting more than one parathyroid gland
- Parathyroid carcinoma.
Primary hyperparathyroidism does not usually run in families. However, in a very small number of people, it can be the result of an inherited condition called familial isolated hyperparathyroidism.
Secondary Hyperparathyroidism – Secondary hyperparathyroidism is caused by other diseases or deficiencies that are affecting our body. These other conditions are ones that cause a long-standing, low level of calcium in our blood. Some of the causes of secondary hyperparathyroidism include:
- Chronic kidney disease (CKD)
- Vitamin D deficiency (rickets/osteomalacia)
- Gut (intestinal) malabsorption
Tertiary Hyperparathyroidism – This type of hyperparathyroidism occurs as a result of long-standing secondary hyperparathyroidism. In tertiary hyperparathyroidism, the condition that was causing our low blood calcium level and the secondary hyperparathyroidism has been treated or our blood calcium level has been brought back to normal.
Sign and Symptoms of Hyperparathyroidism
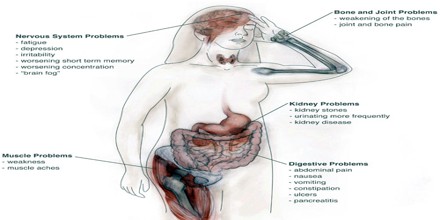
In primary hyperparathyroidism about 75% of people have no symptoms. The problem is often picked up during blood work for other reasons via a raised calcium. Many other people only have non-specific symptoms. Symptoms directly due to hypercalcemia are relatively rare, being more common in patients with malignant hypercalcemia.
Some symptoms may include: fatigue, weakness, depression, body aches, appetite loss, constipation, vomiting, nausea, excessive thirst, increased urination, confusion, memory problems, and kidney stones.
In secondary hyperparathyroidism the parathyroid gland is behaving normally; clinical problems are due to bone resorption and manifest as bone syndromes such as rickets, osteomalacia and renal osteodystrophy.
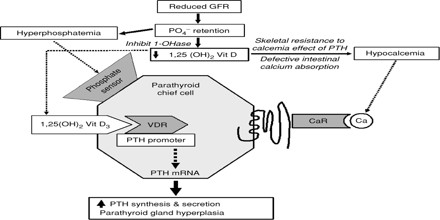
Mechanism of Hyperparathyroidism
Normal parathyroid glands measure the ionized calcium (Ca2+) concentration in the blood and secrete parathyroid hormone accordingly: if the ionized calcium rises above normal the secretion of PTH is decreased, whereas when the Ca2+ level falls, parathyroid hormone secretion is increased. Secondary hyperparathyroidism involves increases in PTH gene expression, synthesis, and secretion, and if chronic, to proliferation of the PT cells. Low serum Ca2+ leads to an increase in PTH secretion, PTH mRNA stability, and PT cell proliferation. Pi also regulates the PT in a similar manner. The effect of Ca2+ on the PT is mediated by a membrane Ca2+receptor. 1, 25(OH) 2D3 decreases PTH gene transcription.