Secondary Hyperparathyroidism
Definition
Secondary Hyperparathyroidism is a disease of the parathyroid glands that was caused by some other disease. The parathyroid glands grew big and went crazy “secondary” to some other problem. It means the parathyroid glands are overproducing parathyroid hormone in an attempt to help the body increase the amount of calcium in the blood. It is the only job of the parathyroid glands to maintain normal calcium levels and the four parathyroid glands will increase the production of their hormone (Parathyroid Hormone, or PTH) if the calcium is too low.
Secondary Hyperparathyroidism cannot ever be associated with high blood calcium. Even a slightly high calcium level excludes the possibility of secondary hyperparathyroidism. Thus if our calcium level is 10.0 mg/dl or higher (2.5 mmol/l or higher for our European friends) weu cannot have secondary hyperparathyroidism.
Secondary Hyperparathyroidism only occurs in a few situations where a patient cannot absorb enough calcium in their diet, or they have kidney failure requiring dialysis and they lose control of calcium and phosphorus. Because it is the primary and only job of the parathyroid glands to help maintain calcium in the normal range, a low calcium level will cause all four parathyroid glands to produce more parathyroid hormone (PTH) in an attempt to increase calcium absorption in the intestines, and to remove calcium out of the bones.
Causes of Secondary Hyperparathyroidism
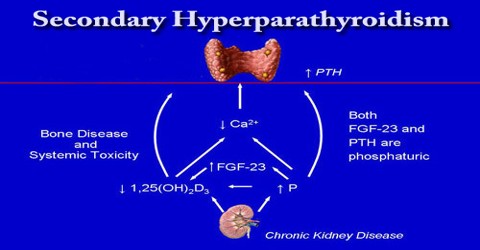
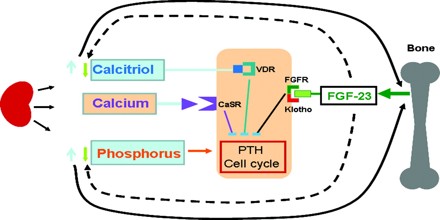
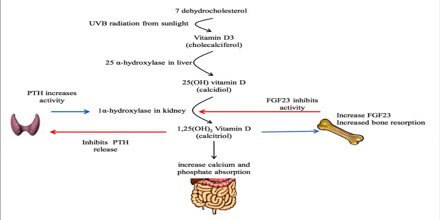
There are only a few causes of secondary hyperparathyroidism. In addition to kidney failure, there are a few causes of secondary hyperparathyroidism which are associated with poor absorption of calcium by the intestines, leading to low normal or low blood calcium. The parathyroid glands help control calcium use and removal by the body. They do this by producing parathyroid hormone, or PTH. PTH helps control calcium, phosphorus, and vitamin D levels within the blood and bone. It is usually caused by kidney failure, a problem where the kidney is unable to clean the blood of phosphorus produced by the body and unable to make enough vitamin D, specifically calcitriol, the active form of vitamin D.
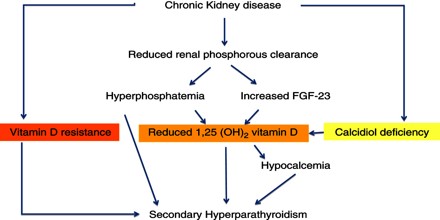
Other less common causes of secondary hyperparathyroidism are long-term lithium therapy, vitamin D deficiency, gastrointestinal malabsorption syndromes, when the intestines do not absorb vitamins and minerals properly, malnutrition, vitamin D-resistant rickets, or hypermagnesemia (abnormally high blood magnesium levels). Calciphylaxis is uncommon. These painful skin lesions begin as small nodules or plaques with a purplish color, mottling, or livedo reticularis in a stellate pattern. The ulcers grow and parts become necrotic (i.e. the tissue dies). They rarely heal with routine wound care measures.
Sign and Symptom of Secondary Hyperparathyroidism
General symptoms may include:
- Bone deformities
- Broken bones (fractures)
- Swollen joints
Other symptoms relate to the underlying cause of secondary hyperparathyroidism.
- Chronic kidney failure
- Malabsorption
- Rickets
Diagnosis and Treatment of Secondary Hyperparathyroidism
The Parathyroid Hormone or PTH is elevated due to decreased levels of calcium or 1, 25-dihydroxy-vitamin D3. It is usually seen in cases of chronic kidney disease or defective calcium receptors on the surface of parathyroid glands.
Correcting the calcium level and the underlying problem can bring the PTH levels back to normal.
Treatment may involve:
- A special form of vitamin D (requires a doctor’s prescription) if anyone have low vitamin D levels
- Surgery for cancer
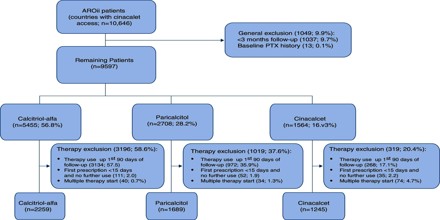
- Patients with chronic kidney failure are usually given calcium and vitamin D, and are told to avoid phosphate in their diet. A medication called cinacalcet (Sensipar) may also be recommended. Dialysis, a kidney transplant, or parathyroid surgery may be needed.
- Most people with hyperparathyroidism secondary to chronic kidney disease will improve after renal transplantation, but many will continue to have a degree of residual hyperparathyroidism (tertiary hyperparathyroidism) post-transplant with associated risk of bone loss, etc.
Prevention of Secondary Hyperparathyroidism
Early diagnosis and treatment of rickets or vitamin D deficiency may prevent this condition. Proper treatment of kidney failure helps reduce symptoms of secondary hyperparathyroidism.