Synthetic protein-based nanoparticles that simultaneously strengthen and suppress the immune system’s reactivity. The condition known as sepsis, in which the immune system is highly dysregulated, may be treated using this technology.
In order to create and test a novel new nanomedicine, immunologists at Radboud University Medical Center (Radboudumc) and bioengineers from the Eindhoven University of Technology (TU/e) have teamed up. Their research results have just been published in Nature Biomedical Engineering.
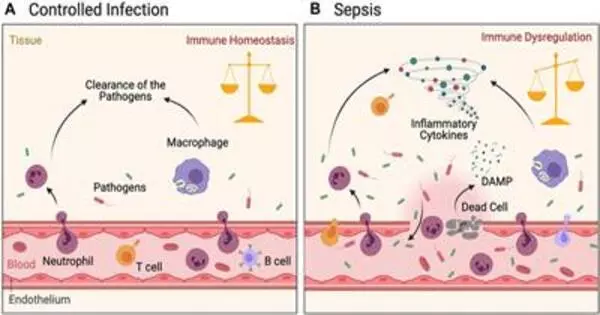
The immune system becomes dysregulated in sepsis, a potentially fatal illness, as a result of an infection with a bacteria, fungus, or virus. Hyperinflammation, an excessively strong immune response, can result from this imbalance. As a result, tissues are damaged and organs fail.
The immune system can also exhaust itself simultaneously, sometimes to the point of paralysis. Immune paralysis is what causes the body to become susceptible to a fresh infection.
Joining forces
Researchers from all over the world have been looking for a sepsis treatment for years. Such a therapy requires a medicine that simultaneously combats the immune system’s response and paralysis. A huge risk, though, is that a potential medication to prevent that overreaction might instead cause paralysis.
We have been developing new proteins by fusing body proteins for some time. We did the same for interleukin-4. We made nanoparticles of it. By injecting these nanoparticles into the bloodstream, interleukin-4 is delivered to the target cells.
Professor Willem Mulder
In a petri dish containing immune cells, immunologists from the Radboudumc center found that the cytokine interleukin-4 inhibits inflammation while unexpectedly inducing trained immunity. This paradoxical feature may be utilized to treat sepsis, but it requires that interleukin-4 is targeted to immune cells in the human body.
On the technological front, researchers at TU/e have a lot of expertise in creating cutting-edge nanotechnology-based methods to treat cancer, for instance.
In light of their various studies, TU/e bioengineers created a novel nanotechnology-based strategy by fusing interleukin-4 with a protein that ordinarily generates nanoparticles with lipid molecules.
Small fat particles
A novel form of nanomedicine was created by researchers, consisting of tiny fat particles made from natural proteins that interact very selectively with immune cells. In this instance, interleukin-4 and another body protein were fused to create a novel protein that integrates into fat particles.
As a result, interleukin-4 is delivered specifically to immune cells, reducing the acute inflammatory response and enhancing the immune system at the same time. Thus, the immune system is balanced.
Mihai Netea, professor of Experimental Internal Medicine at Radboudumc, says “We know that the protein interleukin-4 counteracts an overreaction of the immune system. We were surprised that in a test tube this protein could also trigger trained immunity in certain immune cells.”
Our innate immune system’s trained immunity is the portion that can learn new things, which makes our immune system stronger. TU/e created a new nanomedicine based on interleukin-4 to do that in people. According to the outcomes, it was effective. The immune system was restored by the nanoparticles in both laboratory animals and blood samples from sepsis patients.
New technology
The researchers’ use of this nanotechnology was novel since they were able to target interleukin-4 to particular immune cells. Willem Mulder, professor of Precision Medicine at both Radboudumc and TU/e, says “We have been developing new proteins by fusing body proteins for some time. We did the same for interleukin-4. We made nanoparticles of it. By injecting these nanoparticles into the bloodstream, interleukin-4 is delivered to the target cells.”
The researchers stress that the therapy has not yet been tested in patients. Follow-up research is needed for this. Nevertheless, the approach is a very cutting-edge type of immunotherapy that opens up new therapeutic options for the treatment of sepsis, a condition that claims the lives of over 3,500 people yearly in the Netherlands alone.
Mulder and Netea founded the biotech incubator BioTrip in collaboration with drug developers and biotech investors to bring the newest technology to patients.
“We don’t want this exciting technology to end with our beautiful publication, which often happens in academia. Through BioTrip, we have a pathway for clinical translation. Hopefully, our work and joint efforts will ultimately lead to a therapeutic that can help decrease the high mortality and morbidity rates in sepsis,” adds co-author and dean of TU/e’s Department of Biomedical Engineering Professor Maarten Merkx.