INTRODUCTION:
Urinary incontinence, the loss of bladder control is a common and often embarrassing problem. The severity of urinary incontinence ranges from occasionally leaking urine when cough or sneeze to having sudden, unpredictable episodes of strong urinary urgency. Sometimes, the urgency may be so strong don’t get to a toilet in time.
Quality of life is significantly diminished in women with urinary incontinence. Alterations in daily activities and social disengagement are common by-products of the condition. Unfortunately, many patients with urinary incontinence do not seek the help of health care providers because of embarrassment or the incorrect belief that it is a normal part of aging which cannot be treated. And frequently, when patients do discuss the problem with their physician, these misconceptions are reinforced.
Although urinary incontinence affects millions of people, it isn’t a normal part of aging or, in women, an inevitable consequence of childbirth or changes after menopause. It’s a medical condition with many possible causes, some relatively simple and self-limited and others more complex.
Incontinence can affect persons at any age; however women over 50 are the most common sufferers and younger women who have just given birth. Approximately 50% of older adults are currently institutionalized due to urinary incontinence. On average, one in four adult women has experienced urinary incontinence at some point in their life. There are many causes of incontinence. Some of these causes include pregnancy, childbirth, and hormone changes during the menopausal years.
Incontinence is very common, but not a condition that should be ignored. Eight out of ten times continence can be improved through exercise, biofeedback or surgical intervention.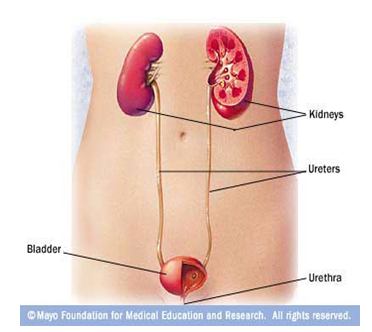
IN WOMEN, THE URETHRAL OPENING IS LOCATED JUST ABOVE THE VAGINA:
IN MEN, THE URETHRAL OPENING IS AT THE TIP OF THE PENIS:
Urinary and bladder control is dependent on activities coordinated between the smooth muscle tissue of the urethra and bladder, skeletal muscle, voluntary inhibition, and the autonomic nervous system. The kidneys filter and cleanse the blood to produce urine, which is stored in the bladder. Nerves in the bladder tell the brain when the bladder is filled with urine resulting in the urge to urinate. Once on the toilet, brain signals the urethra sphincter muscles to relax while signaling the bladder muscles to contract, thus releasing urine.
Changes with age can reduce how much urine one’s bladder can hold. Aging can make one’s stream of urine weaker and can cause one to feel the urge to urinate more often. This doesn’t mean one’ll have urinary incontinence just because one is aging. With treatment it can be controlled or cured.
This long-term prospective observational study describes thenatural progression of urinary incontinenceafter first delivery and suggests a strong association betweenvaginal delivery and increasing prevalence of stress urinary incontinence symptoms 10 years after thefirst delivery. Although the majority of symptomatic patientsin experienced mild to moderate complaints, the incidencerate of urinary incontinence episodes increased five to sixtimes after vaginal delivery.
Anal sphincter rupture, perineal tears or instrumental deliveryused as a proxy for severe obstetric trauma to the lower urinarytract did not correlate with the presence of urinary incontinence10 years after the first delivery. Instrumental delivery hasbeen shown to have injurious urinary tract side-effects in prospectivestudies; however, the detrimental effects of vaginal deliverymay not be limited to tears or ruptures of supportive tissues.Instead our data support the considerable evidence indicatingthat nondisruptive tissue trauma to the pelvic floor may bea major contributor to the complicated, and multifactor,pathoetiologic mechanisms behind stress urinary incontinenceand other pelvic floor disorders.This may be explained bystretching of the tissues or ischemic trauma to the distal branchesof the pudendal nerve, causing enervation of the intrinsicurethral sphincter.
Age and degenerative changes of the bladder are often promotedas key risk factors for urinary incontinence. However, in thispresumed premenopausal population, age at the time of firstdelivery was not associated with an increased risk of urinaryincontinence or urgency. The pattern and distribution of urinaryurgency was similar to that of stress urinary incontinence,showing pronounced adverse alterations after the first deliverycompared with baseline. These data make us conclude, that althoughthe disease mechanisms of urinary urgency differ from thoseof stress urinary incontinence, vaginal delivery seems to havea major effect on the prevalence of urgency as well. One mayspeculate that nondisruptive tissue trauma, especially nervedamage, may have a more pronounced effect on de novo urgencysymptoms.
The most dramatic changes in bladder function were observedin the range of mild-moderate symptoms. This was reflected bythe low rate of surgical interventions over the study period.We could not confirm that maternal age at the time of firstdelivery was associated with an increased risk for urinary incontinencesurgery, as has been suggested.Future life events such asmenopausal estrogen depletion and periurethral atrophy may,however, cause symptoms to worsen and increase demands forsurgical correction later in life.
Stressurinary incontinence is, however, a disorder defined by self-experiencedsymptoms, and the predictive value of urodynamic investigationsis limited in stress urinary incontinence.
Urinary incontinence also exists in nulliparous women, and werecognize that other factors, such as a hereditary predisposition, menopausal loss of estrogen, and pelvic surgery, may havea major influence on the development of bladder and urinarydysfunction. Thus, the development of urinary incontinence islikely to be multifactor, and the lack of a nonporous controlgroup is an obstacle when trying to isolate the effects of ageing.It is, however, implausible that the observed alterations inlower urinary tract function should be attributed to the ageingprocess, because most of the adverse effects were apparent already6–9 months after the index delivery. Furthermore, in thiscohort of healthy women, most subjects would be premenopausal10 years after their first delivery, and none had undergoneother life events associated with lower urinary tract dysfunction,such as hysterectomy, pelvic organ prolapsed surgery, or pelvicorgan radiotherapy.
DEFINITION:
Urinary Incontinence is the involuntary excretion of urine from one’s body. It is often temporary, and it almost always results from an underlying medical condition. Frequent urination, which may or may not be a symptom of underlying pathology, is not synonymous with urinary incontinence. Urinary Incontinence, also called Overactive bladder.
Urinary incontinence (UI) is the loss of urine control, or the inability to hold urine until can reach a restroom. Urinary incontinence may be a temporary condition, resulting from an underlying medical condition. It can range from the discomfort of slight losses of urine to severe, frequent wetting.
Incontinence is the inability to control the passage of urine. This can range from an occasional leakage of urine, to a complete inability to hold any urine.
Urinary incontinence is unintentional loss of urine that is sufficient enough in frequency and amount to cause physical and/or emotional distress in the person experiencing it.
Incontinence is a problem of the urinary system, which is composed of two kidneys, two greeters, a bladder, and a urethra. The kidneys remove waste products from the blood and continuously produce urine. The muscular, tube-like ureters move urine from the kidneys to the bladder, where it is stored until it flows out of the body through the tube-like urethra. A circular muscle, called the sphincter, controls the activity of the urethra. It is not a part of the urinary incontinence.
KEGELS EXERCISE : An exercise developed by Dr. Arnold Kegel to strengthen the muscles of the pelvic floor — especially the pubococcygeal (PC) muscles — to increase vaginal muscle tone, improve sexual response, and limit involuntary urine release due to stress urinary incontinence.
CLASSIFICATION
Types of Incontinence:
- Long-term (chronic) incontinence usually starts gradually and slowly becomes worse. Incontinence is the involuntary loss of urine. It is not a disease but a symptom of a problem with the urinary tract.
- Acute Incontinence is a temporary loss of urine control that ends when the problem causing it is successfully treated. It may be caused by childbirth, urinary tract infection, drug side effect, constipation or bladder stones.
Chronic incontinence is a long-term loss of urine control. It may be caused by muscle weakness in the urinary tract or by damage or malfunction in the urinary tract or the nerves that control urination. It is common for a person to have more than one cause of incontinence. Chronic incontience is more common in women than in men. Chronic can be classified into several types. These are the most common types:
There are four major types of Incontinence:
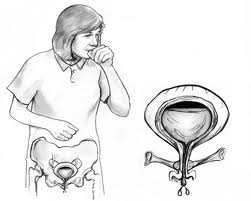
- Stress incontinence Urine leaks due to sudden pressure on lower stomach muscles, (i.e. coughing, sneezing, laughing, heaving lifting, exercise), usually as the result of weakened pelvic muscles.
Stress incontinence is when urine leaks because of sudden pressure on lower stomach muscles, such as when cough, laugh, lift something or exercise. Stress incontinence usually occurs when the pelvic muscles are weakened, for example by childbirth or surgery. Stress incontinence is common in women. Stress Incontinence Leakage with cough, sneeze, exercise, activity.
STRESS INCONTINENCE IS AN INVOLUNTARY LOSS OF CONTROL OF URINE THAT OCCURS AT THE SAME TIME ABDOMINAL PRESSURE IS INCREASED AS IN COUGHING OR SNEEZING. ITDEVELOPS WHEN THE MUSCLES OF THE PELVIC FLOOR HAVE BECOME WEAK
Stress incontinence is incontinence that is caused by actions such as coughing, laughing, sneezing, exercising or other movements that increase intrabdominal pressure and thus increase pressure on the bladder. Physical changes resulting from pregnancy, childbirth, and menopause often cause stress urinary incontinence. It is the most common form of urinary incontinence in women and is treatable .
The bladder is supported by muscles of the pelvic floor. If these muscles weaken, the bladder can move downward, pushing slightly out of the bottom of the pelvis toward the vagina. This prevents muscles that ordinarily force the urethra shut from squeezing as tightly as they should. As a result, urine can leak into the urethra during moments of physical stress. Stress incontinence also occurs if the muscles that do the squeezing weaken.
Stress urinary incontinence can worsen during the week before the menstrual period. At that time, lowered estrogen levels might lead to lower muscular pressure around the urethra, increasing chances of bladder leakage. The incidence of stress incontinence increases following menopause.
- Urge incontinence
- Urine leaks because of the sudden urge to urinate, before reach the toilet.
This occurs when the need to urinate comes on too fast — before get to a toilet. Body may only give a warning of a few seconds to minutes before urinate. Urge incontinence is most common in the elderly and may be a sign of an infection in the kidneys or bladder. Urge Incontinence Leakage with the urgent desire to void.
Urge urinary incontinence is involuntary loss of urine occurring for no apparent reason while suddenly feeling the need or urge to urinate. The most common cause of urge incontinence is inappropriate bladder contractions.
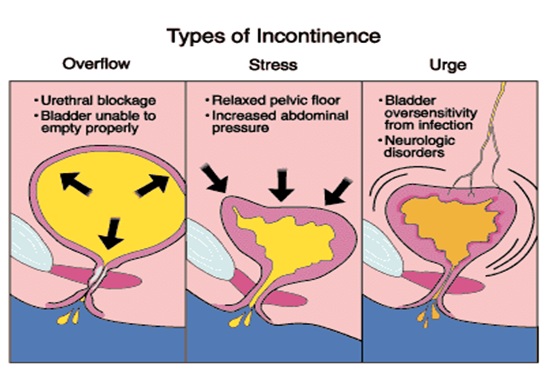
Overflow incontinence:
- Urine leaks because the bladder is overfilled but doesn’t send the signal to the brain to urinate.
This type of incontinence is a constant dripping of urine. It’s caused by an overfilled bladder. This often occurs in men and can be caused by something blocking the urinary flow, such as an enlarged prostate gland or tumor. Diabetes or certain medicines may also cause the problem. Overflow Incontinence Leakage associated with overdistended bladder.
Overflow urinary incontinence occurs when the patient’s bladder is always full so that it frequently leaks urine. Weak bladder muscles or a blocked urethra can cause this type of incontinence. Nerve damage from diabetes or other diseases can lead to weak bladder muscles; tumors and urinary stones can block the urethra. Overflow incontinence predominately affects men.
- Functional incontinence Urine leaks not due to a urinary condition but due to a physical disability or mobility issue slowing down a person’s ability to get to the toilet in time.
This type occurs when you have normal urine control but have trouble getting to the bathroom in time. The patient may not be able to get to the bathroom because of arthritis or other diseases that make it hard to move around. Functional Incontinence Leakage due to physical inability to get to bathroom.
People with functional urinary incontinence may have problems thinking, moving, or communicating that prevent them from reaching a toilet. A person with Alzheimer’s disease, for example, may not think well enough to plan a timely trip to a restroom. A person in a wheelchair may be blocked from getting to a toilet in time. Conditions such as these are often associated with age and account for some of the incontinence of elderly men and women in nursing homes.
Other Types of Incontinence:
Mixed Incontinence:
Combination of stress and urge. Stress and urge urinary incontinence often occur together in women. Combinations of incontinence – and this combination in particular – are sometimes referred to as “mixed urinary incontinence.”
“Transient incontinence” is a temporary version of incontinence. It can be triggered by medications, urinary tract infections, mental impairment, restricted mobility, and stool impaction (severe constipation), which can push against the urinary tract and obstruct outflow.
Reflex incontinence:
The loss of urine when the person is unaware of the need to urinate may result from an abnormal opening between the bladder and another structure or from a leak in the bladder, urethra or ureter. Incontinence from surgery follows such operations as hysterectomies, caesarean sections, prostatectomies, lower intestinal surgery, or rectal surgery.
Anatomical incontinence:
It results when there are problems with the urinary tract that affect the urine flow. They may be present from birth.
De-estrogenization of the urethra occurs with the loss of estrogen after menopause. Estrogen makes the urethra spongy, and this imparts increased resistance to the flow of urine.
Paradoxical incontinence:
Occurs with mechanical or functional urethral obstruction. When bladder pressure exceeds pressure at the site of obstruction, urine leaks past the obstruction.
Urethral sphincter incompetence:
Decreased urethral sphincter tone leading to stress incontinence, urine leakage at rest, or urine leakage with activity. Hormone-responsive incontinence is one type of urethral sphincter incompetence.
ETIOLOGY:
Urinary incontinence can be caused by many different medical problems, including weak pelvic muscles or diabetes.
Causes of urinary incontinence:
- For women, thinning and drying of the skin in the vagina or urethra, especially after menopause. For men enlarged prostate gland or prostate surgery.
- Weakened pelvic muscles.
- Certain medicines.
- Build-up of stool in the bowels.
- Not being able to move around.
- Urinary tract infection. Problems such as diabetes or high calcium levels.
Transient Causes of Incontinence:
- Delirium
- Infection
- Atrophic vaginitis/urethritis
- Pharmaceuticals/psychological
- Endocrine (DM)
- Restricted mobility
- Stool impaction
The most common kind of urinary incontinence in women is stress incontinence. It causes urine to leak during lifting, exercise, coughing, sneezing, or laughing. Stress incontinence is caused by relaxed pelvic muscles that may have been stretched or torn during child-bearing.
Incontinence may be caused or made worse by problems such as:
- Constipation
- Infection
- A stone in the bladder
- Use of diuretics (“water pills”)
- Thinning of tissue due to decreased estrogen after menopause, which may weaken urethral muscle.
Common Causes:
Incontinence may be sudden and temporary, or ongoing and long-term. Causes of sudden or temporary incontinence include:
- Urinary tract infection or inflammation
- Prostate infection or inflammation
- Stool impaction from severe constipation, causing pressure on the bladder
- Side effects of medications (such as diuretics, tranquilizers, some cough and cold remedies, certain antihistamines for allergies, and antidepressants).
- Increased urine amounts, like with poorly controlled diabetes.
- Pregnancy.
- Weight gain.
- Short-term bedrest — for example, when recovering from surgery.
- Mental confusion.
Causes that may be more long-term:
- Spinal injuries.
- Urinary tract anatomical abnormalities.
- Neurological conditions like multiple sclerosis or stroke.
- Weakness of the sphincter, the circular muscles of the bladder responsible for opening and closing it; this can happen following prostate surgery in men, or vaginal surgery in women. Pelvic prolapse in women — falling or sliding of the bladder, urethra, or rectum into the vaginal space, often related to having had multiple pregnancies and deliveries.
- Large prostate in men.
- Depression or Alzheimer’s disease.
- Nerve or muscle damage after pelvic radiation.
- Bladder cancer.
- Bladder spasms.
Causes of temporary urinary incontinence:
Certain foods, drinks and medications can cause temporary urinary incontinence. A simple change in habits can bring relief.
- Alcohol. Beer, wine and spirits are all diuretics. They cause bladder to fill quickly, triggering an urgent and sometimes uncontrollable need to urinate. In addition, alcohol can temporarily impair ability to recognize the need to urinate and act on that need in a timely manner.
- Ver-hydration. Drinking a lot of water or other beverages, particularly in a short period of time, increases the amount of urine bladder has to deal with and may result in an occasional accident.
- Dehydration. If urge incontinence, may try to limit fluids to reduce the number of trips to the toilet. However, if don’t consume enough liquid to stay hydrated, urine can occasionally become very concentrated. This collection of concentrated salts can irritate bladder and worsen urge incontinence.
- Caffeine. Caffeine also is a diuretic. It causes bladder to fill more quickly and hold less than usual so that suddenly and perhaps uncontrollably need to urinate.
- Bladder irritation. Carbonated drinks, tea and coffee — with or without caffeine — may irritate bladder and cause episodes of urge incontinence. Citrus fruits and juices and artificial sweeteners also can be sources of aggravation.
- Medications. Sedatives, such as sleeping pills, can sometimes interfere with ability to control bladder function. Other medications — including water pills (diuretics), muscle relaxants and antidepressants — can cause or increase incontinence. Some high blood pressure drugs, heart medications and cold medicines also can affect bladder function. After surgery, some people experience temporary overflow incontinence from the lingering effects of anesthesia.
- Other illnesses or injuries. Any serious illness, injury or disability that keeps from getting to the toilet in time also is a potential cause of incontinence.
Causes of persistent urinary incontinence:
- Pregnancy and childbirth. Pregnant women may experience stress incontinence because of hormonal changes and the increased weight of an enlarging uterus. In addition, the stress of a vaginal delivery can weaken the pelvic floor muscles and the ring of muscles that surrounds the urethra (urinary sphincter). The result is often stress incontinence — urine escapes past the weakened muscles whenever pressure is placed on bladder. The changes that occur during childbirth can also damage bladder nerves and supportive tissue and can lead to a dropped (prolapsed) pelvic floor, producing a vaginal bulge.
With prolapse, bladder, uterus, rectum or small bowel can get pushed down from the usual position and protrude into your vagina. Such protrusions can be associated with incontinence. Incontinence related to childbirth may develop right after delivery or, more likely, may not develop until years later.
- Changes with aging. Aging of the bladder muscle affects both men and women, leading to a decrease in the bladder’s capacity to store urine and an increase in overactive bladder symptoms. Risk of overactive bladder increases if have blood vessel disease, so maintaining good overall health — including stopping smoking, treating high blood pressure and keeping weight within a healthy range — can help curb symptoms of overactive bladder.
- Women produce less of the hormone estrogen after menopause, a decrease that can contribute to incontinence. Estrogen helps keep the lining of the bladder and urethra healthy. With less estrogen, these tissues lose some of their ability to close — meaning that urethra can’t hold back urine as easily as before.
- Hysterectomy. In women, the bladder and uterus (womb) lie close to one another and are supported by the same muscles and ligaments. Any surgery that involves a woman’s reproductive system — for example, removal of the uterus (hysterectomy) — runs the risk of damaging the supporting pelvic floor muscles, which can lead to incontinence.
- Painful bladder syndrome (interstitial cystitis). This rare, chronic condition can be associated with an inflammation of the bladder wall. It occasionally causes urinary incontinence, as well as painful and frequent urination. Interstitial cystitis affects women more often than men, and its cause isn’t clear.
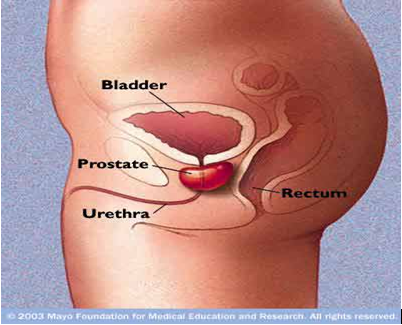
- Prostatitis. Loss of bladder control isn’t a typical sign of prostatitis, or inflammation of the prostate gland — a walnut-sized organ located just below the male bladder. Even so, urinary incontinence sometimes occurs with this extremely common condition. The prostate actually surrounds the urethra, so inflammation of the prostate occasionally swells and constricts the urethra, blocking normal urine flow and leading to urinary urgency and frequency. Rarely, this also causes incontinence.
- Enlarged prostate. In older men, incontinence often stems from enlargement of the prostate gland, a condition also known as benign prostatic hyperplasia (BPH). The prostate begins to enlarge in many men after about age 40. As the gland enlarges, it can constrict the urethra and block the flow of urine. For some men, this problem results in urge or overflow incontinence.
- Prostate cancer. In men, stress incontinence or urge incontinence can be associated with untreated prostate cancer. However, more often, incontinence is a side effect of treatments — surgery or radiation — for prostate cancer.
- Bladder cancer or bladder stones. Incontinence, urinary urgency and burning with urination can be signs and symptoms of bladder cancer and also of bladder stones. Other signs and symptoms include blood in the urine and pelvic pain.
- Neurological disorders. Multiple sclerosis, Parkinson’s disease, stroke, a brain tumor or a spinal injury can interfere with nerve signals involved in bladder control, causing urinary incontinence.
- Obstruction. A tumor anywhere along urinary tract can obstruct the normal flow of urine and cause incontinence, usually overflow incontinence. Urinary stones — hard, stone-like masses that can form in the bladder — may be to blame for urine leakage. Urinary obstruction can also occur after overcorrection during a surgical procedure to correct urinary incontinence, leading to more urine leakage.
Review of a voiding diary from the patient:
- Urine analysis – looking for blood, stone crystals, bacteria.
- Urine culture – looking for an infection.
- Urine cytology – looking for cancer cells in the urine.
- IVP – an x-ray looking at the kidneys, the urine tubes that connect the kidney to the bladder (ureters), and the bladder.
- Kidney Ultrasound – looking at the kidneys.
- Bladder ultrasound – looking at the bladder.
- Cystoscopy – looking into the bladder with a small scope that has a miniature camera on the tip.
- Urodynamics – a test that involves putting a small tube into the rectum and a small tube into the bladder and taking measurements during bladder filling and emptying.
Stress incontinence can be caused by:
- Lack of function of the sphincter that normally helps to hold back urination.
- Weakness of the muscles that support the urethra and bladder.
Urologist can determine the cause of stress incontinence with a few tests including:
- Health history and physical exam.
- Urodynamics – a test that involves putting a small tube into the rectum and a small tube into the bladder and taking measurements during bladder filling.
Neurologic causes of incontinence:
Urinary incontinence is often associated with neurologic disease. Neurologic abnormalities may disrupt function of the detrusor muscle, urethral sphincters, or both. Neurologic incontinence may result from trauma, tumors, or herniated intervertebral discs. The location of the lesion will dictate the type of micturition disorder and other concurrent neurologic abnormalities. Upper motor neuron (UMN) lesions are those above the sacral spinal cord segments (L5 in the dog and L7 in the cat); lower motor neuron (LMN) lesions involve the sacral segments.
Patients with UMN lesions lack voluntary control of micturition. Urination may be initiated by spinal reflexes, but an absence of sensation and central control, and the sphincters’ failure to relax lead to interrupted, involuntary, and incomplete voiding. Manual bladder expression is difficult if sphincter tone is increased, but the urethra can be catheterized normally. Overflow of urine occurs when the bladder pressure exceeds sphincter resistance. The perineal reflex is intact.
Detrusor areflexia with decreased sphincter tone is a result of disease of the sacral spinal cord or bilateral lesions of the sacral spinal nerve roots (LMN lesions). Voluntary control of urination is absent. Tail paralysis and fecal incontinence may be present. The perineal reflex and bulbospongiosus reflexes are absent. The bladder is easily expressed, and dribbling of urine occurs when intravesicular pressure exceeds urethral pressure.
Detrusor areflexia can occur secondary to prolonged overdistention of the bladder. Tight junctions between muscle cells are disrupted, preventing spread of nerve impulses. The animal will attempt to void because sensory pathways are intact, but the atonic, flaccid bladder is unable to contract. Residual urine volume is large.
Reflex dyssynergia occurs with incomplete spinal cord lesions cranial to the sacral spinal cord segments. The detrusor reflex is normal to hyperactive, and the urethral sphincters are hyperactive. The patient voluntarily initiates urination, but the urine stream is abruptly stopped because there is lack of synchronization between bladder contraction and urethral relaxation, leading to incomplete voiding. Urethral obstruction can result in a similar pattern of micturition.
Nonneurologic causes of incontinence:
Urinary incontinence in young animals may be congenital, whereas the condition is usually acquired in older animals. Congenital abnormalities resulting in urinary incontinence include ectopic ureters, patent urachus, female pseudohermaphroditism, rectovaginal fistula, and vestibulovaginal stenosis.
The most common congenital anomaly of the urinary tract is ectopic ureters. Scientist has a higher prevalence of this abnormality than do other breeds. Although recognized primarily in female dogs, male dogs and cats of both sexes can be affected. The condition is rare in the cat, with a higher prevalence in males. If the condition is unilateral, the animal can urinate normally in addition to dribbling urine. If both ureters bypass the bladder, the animal may only dribble urine and not be able to urinate normally. The diagnosis of ectopic ureters may be made with contrast urography, contrast vaginourethrography, or direct visualization using cystoscopy/ vaginoscopy. Surgical correction can be curative, or the animal may remain incontinent despite surgery because of the presence of other anatomic congenital abnormalities of the lower urinary tract.
Several acquired disorders of the urinary tract can result in incontinence. Chronic cystitis resulting in fibrosis, partial cystectomy, or postsurgical adhesions to the bladder can reduce bladder capacity, resulting in urge incontinence. A frequent, uncontrollable desire to void may be confused with urethral incontinence. Severe urethral inflammation can decrease sphincter tone and result in incontinence. Urethral calculi or luminal or extraluminal masses can interfere with normal urination and cause incontinence when intravesicular pressure exceeds urethral pressure at the site of the obstruction. This is called paradoxical incontinence.
RISK FACTORS:
- Gender
Women are more likely than men are to have stress incontinence. Pregnancy and childbirth, menopause, and normal female anatomy account for this difference. However, men with prostate gland problems are at increased risk of urge and overflow incontinence.
- Age
As you get older, the muscles in your bladder and urethra lose some of their strength. Changes with age reduce how much your bladder can hold and increase the chances of involuntary urine release. However, getting older doesn’t necessarily mean that you’ll have incontinence. Incontinence isn’t normal at any age — except during infancy.
- Obesity
Being overweight increases the pressure on your bladder and surrounding muscles, weakening them and allowing urine to leak out when you cough or sneeze.
- White or Japanese extraction.
- Episiotomy, third- and fourth-degree perineal lacerations.
- Exposure to oxytocin in labor.
- Prolonged labor.
- Prolonged second stage of labor.
- Giving birth to a large infant.
- Instrumented delivery.
- Obstructed labor with pressure-related necrosis of bladder base and proximal urethra (rare in developed countries).
- The pregnant state itself (ie, apart from delivery).
- Smoking
A chronic cough can cause episodes of incontinence or aggravate incontinence that has other causes. Constant coughing puts stress on your urinary sphincter. Longtime smokers often experience stress incontinence for this reason. Smokers are also at risk of developing overactive bladder.
- Vascular disease
People with extensive vascular disease that can occur with aging are at increased risk of overactive bladder.
- Participating in high-impact sports
High-impact sports — such as running, basketball and gymnastics — can cause episodes of incontinence in otherwise healthy women. These vigorous activities put sudden, strong pressure on your bladder, allowing urine to leak past your urinary sphincter. However, no data links high-impact sports to an increased risk of chronic stress incontinence.
ANATOMY
LEVATOR ANI
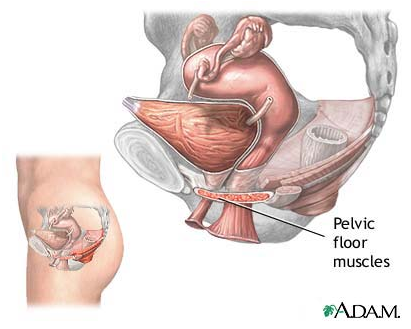
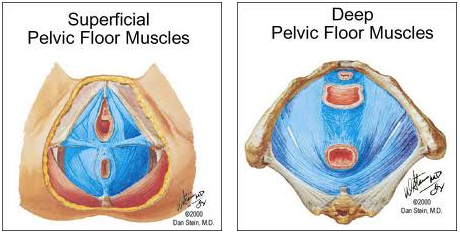
The levator ani is a broad, thin muscle, situated on the side of the pelvis.
It is attached to the inner surface of the side of the lesser pelvis, and unites with its fellow of the opposite side to form the greater part of the floor of the pelvic cavity.
It supports the viscera in pelvic cavity, and surrounds the various structures which pass through it.
In combination with the coccygeus muscle, it forms the pelvic diaphragm.
Origin and insertion of fibers:
The levator ani arises, in front, from the posterior surface of the superior ramus of the pubis lateral to the symphysis; behind, from the inner surface of the spine of the ischium; and between these two points, from the obturator fascia.
Posteriorly, this fascial origin corresponds, more or less closely, with the tendinous arch of the pelvic fascia, but in front, the muscle arises from the fascia at a varying distance above the arch, in some cases reaching nearly as high as the canal for the obturator vessels and nerve.
The fibers pass downward and backward to the middle line of the floor of the pelvis; the most posterior are inserted into the side of the last two segments of the coccyx; those placed more anteriorly unite with the muscle of the opposite side, in a median fibrous raphé (anococcygeal raphé), which extends between the coccyx and the margin of the anus.
The middle fibers are inserted into the side of the rectum, blending with the fibers of the Sphincter muscles; lastly, the anterior fibers descend upon the side of the prostate to unite beneath it with the muscle of the opposite side, joining with the fibers of the sphincter ani externus and transversus perinei, at the central tendinous point of the perineum.
The anterior portion is occasionally separated from the rest of the muscle by connective tissue.
From this circumstance, as well as from its peculiar relation with the prostate, which it supports as in a sling, it has been described as a distinct muscle, under the name of Levator prostatæ.
In the female the anterior fibers of the Levator ani descend upon the side of the vagina.
Innervation:
The levator ani muscles are mostly innervated by the pudendal nerve, perineal nerve and inferior rectal nerve in concert.[3] In addition, sacral spinal nerves (S3, S4) innervate the muscles directly as well (in ~70% [3] of people). Sometimes (in ~40% [3] of people) the inferior rectal nerve innervates the levator ani muscles independently of the pudendal nerve.
Urinary Tract:
The urinary tract is made up of the kidneys, the ureters, the bladder, and the urethra.
Kidneys: The kidneys are a pair of bean-shaped organs located below the ribs near the middle of the back. They remove waste products from the blood, maintain a balance of electrolytes and other substances in the blood, and produce erythropoietin (hormone that triggers the production of red blood cells in the bone marrow).
Each kidney is composed of about 1 million microscopic “filtering packets” composed of capillaries called glomeruli that remove uremic waste products from the blood and form urine. Each glomerulus connects to a long tube, called a tubule.
Together, the glomerulus and the tubule form a unit called a nephron. Each nephron connects to progressively larger tubular branches, until it reaches a large collection area called the calyx. The calices form the funnel-shaped portion of the upper ureter (renal pelvis).
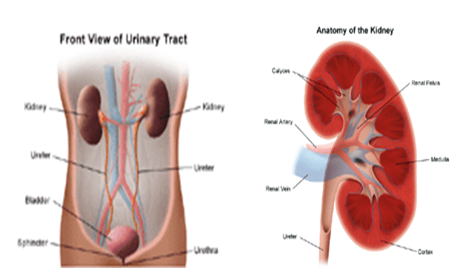
KIDNEY & URINARY SYSTEM PART
Ureters:
The ureters are fibromuscular tubes that convey the urine from the renal pelvis to the bladder. Each ureter is approximately 16 inches long and the one leading from the right kidney is slightly shorter than the left. The ureters consist of mucosal, muscular, and fibrous layers. The area where the ureters enter the bladder is called the trigone. Valves in this region prevent the reflux (i.e., backing up) of urine into the kidneys.
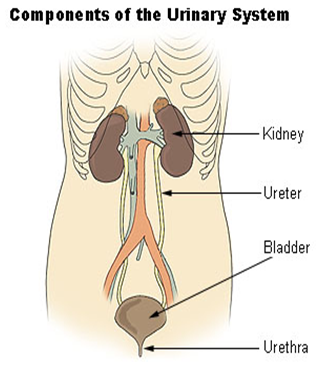
COMPONENT OF URINARY SYSTEM
Bladder:
The urinary bladder is a hollow, muscular organ that stores urine. It is located behind the pubic bone and sits within and is protected by the pelvis. The bladder is held in place by ligaments (bands of tough, fiberlike tissue) that connect it to the pelvis and to other organs. The narrow, internal opening of -the urethra within the bladder is called the bladder neck. Muscles in the bladder neck called sphincters tighten around the urethra to prevent urine from leaking. When the volume of urine in the bladder reaches a certain capacity, the brain sends impulses to the internal sphincter, causing it to relax and to detrusor muscles, causing them to push downward and expel urine. As the bladder contracts, it expels urine out of the body via the urethra.
Studies have documented that about 50% of all women have occasional urinary incontinence, and as many as 10% have frequent incontinence. Nearly 20% of women over age 75 experience daily urinary incontinence.
Stress urinary incontinence is the most common type of urinary incontinence in women. Risk factors for stress incontinence include female sex, advancing age, childbirth, smoking, and obesity. Conditions that cause chronic coughing, such as chronic bronchitis and asthma, may also increase the risk of stress incontinence.
The ability to hold urine and maintain continence is dependent on normal function of the lower urinary tract, the kidneys, and the nervous system. Additionally, the person must possess the physical and psychological ability to recognize and appropriately respond to the urge to urinate.
The process of urination involves two phases:
- The filling and storage phase, and the emptying phase.
- Normally during the filling and storage phase, the bladder begins to fill with urine from the kidneys.
The bladder stretches to accommodate the increasing amounts of urine. The first sensation of the need to urinate occurs when approximately 200 ml of urine is stored. The healthy nervous system will respond to this stretching sensation by alerting you to the need to urinate, while also allowing the bladder to continue to fill.
Urethra:
The urethra is the tube that passes urine from the bladder out of the body. In women, it is approximately 4 centimeters long. It is composed of smooth muscle fibers, sphincter muscle fibers, a layer of elastic tissue, and collagen tissue and is lined with mucous membrane. The female urethra starts at the bladder neck and exits the body directly in front of the vaginal opening (female reproductive canal).
In men, the urethra is roughly 8 to 9 inches long and extends from the bladder neck to the end of the penis. The male urethra is composed of three parts: prostatic, membranous, and spongy. The prostatic urethra is the widest part of the tube and passes through the prostate gland. It is made up of fibrous tissue, muscle fibers, and tiny glandular openings that connect to the prostate. The membranous urethra is approximately three-quarters of an inch long and lies between the triangular ligaments of the pelvis. The spongy urethra is the longest part and extends through the penis to the glans (tip of the penis). The corpus spongiosum is the lower area of the penis that surrounds and protects the urethra.
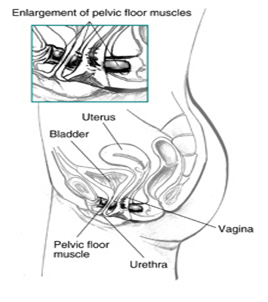
SIDE VIEW OF FEMALE PELVIC MUSCLE
NORMAL URINATION:
The ability to hold urine is dependent on having normal anatomy and a normally functioning urinary tract and nervous system. You must also possess the physical and psychological ability to recognize and appropriately respond to the urge to urinate.
The process of urination involves two phases:
- The filling and storage phase
- The emptying phase
Normally, during the filling and storage phase, the bladder begins to fill with urine from the kidneys. The bladder stretches to accommodate the increasing amounts of urine.
The first sensation of the urge to urinate occurs when approximately 200 ml (just under 1 cup) of urine is stored. A healthy nervous system will respond to this stretching sensation by alerting you to the urge to urinate, while also allowing the bladder to continue to fill
The average person can hold approximately 350 to 550 ml (over 2 cups) of urine. The ability to fill and store urine properly requires a functional sphincter the circular muscles around the opening of the bladder) and a stable, expandable bladder wall muscle (detrusor).
The emptying phase requires the ability of the detrusor muscle to appropriately contract to force urine out of the bladder. At the same time, your body must be able to relax the sphincter to allow the urine to pass out of the body.
Urinary Incontinence & Bladder Control:
Urinary incontinence is surprisingly common. Surgery, medications, childbirth, or injury can interfere with the muscles, nerves and other tissues that work together for bladder control and urinary and rectal function. Middle aged and older people are particularly susceptible to these conditions. But there are a variety of treatments available including exercise programs, medications and surgery. This Special Health Report, Better Bladder and Bowel Control, describes the causes of urinary and bowel or fecal incontinence and treatments tailored to the specific cause
TRANSVERSUS ABDOMINIS MUSCLE
COURSE:
The transversus abdominis muscle, also known as the transversalis muscle and transverse abdominal muscle, is a muscle layer of the anterior and lateral abdominal wall which is medial to (layered below) the internal oblique muscle. It is thought to be a major muscle of the functional core of the human body; although some argue that due to its small cross-sectional area, it cannot generate the forces required to be a prime core stabilize.
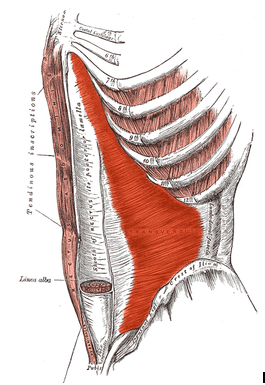
Structure:
The transversus abdominis, so called for the direction of its fibers, is the innermost of the flat muscles of the abdomen, being placed immediately beneath the internal oblique muscle.
Origin
It arises, as fleshy fibers, from the lateral third of the inguinal ligament, from the anterior three-fourths of the inner lip of the iliac crest, from the inner surfaces of the cartilages of the lower six ribs, interdigitating with the diaphragm, and from the lumbodorsal fascia.
Insertion:
The muscle ends anteriorly in a broad aponeurosis, the lower fibers of which curve inferomedially (medially and downward), and are inserted, together with those of the internal oblique muscle, into the crest of the pubis and pectineal line, forming the inguinal aponeurotic falx, also called the conjoint tendon. In layperson’s terminology, the muscle ends in the middle line of a person’s abdomen.
Throughout the rest of its extent the aponeurosis passes horizontally to the middle line, and is inserted into the linea alba; its upper three-fourths lie behind the rectus muscle and blend with the posterior lamella of the aponeurosis of the internal oblique; its lower fourth is in front of the rectus abdominis.
Layman’s description:
- The transverse abs run from our sides (lateral) to the front (anterior), its fibers running horizontally (transverse).
- The lateral beginnings of the muscle (origin) run from the front of the inside part of the hip bone[1] (anterior iliac crest and inguinal ligament) to the last rib of the rib cage. It also is connected to the diaphragm which helps with inhalation.
- The muscle runs transverse and is the deepest of the major abdominal muscles (the others being the rectus abdominis, and the internal and external obliques).
- It ends (the muscle insertion) by joining with the large vertical abdominal muscle in the middle (the linea alba), where the fibers begin to curve downward and upward depending on what direction it has to go to meet the linea alba, and below the sternum it combines with next most superficial muscle (the internal oblique). This insertion runs down by the belly button where it passes over the thick abdomen muscle (the “6/8-pack”) and all the ab muscle fibers join together.
Innervation:
The transversus abdominis is innervated by the lower intercostal nerves (thoracoabdominal, nerve root T7-T11), as well as the iliohypogastric nerve and the ilioinguinal nerve.
Actions:
The transversus abdominis (TVA) helps to compress the ribs and viscera, providing thoracic and pelvic stability. This is explained further here. The transversus abdominis also helps pregnant women deliver their child.
Variations:
It may be more or less fused with the Obliquus internus or absent. The spermatic cord may pierce its lower border. Slender muscle slips from the ileopectineal line to transversalis fascia, the aponeurosis of the Transversus abdominis or the outer end of the linea semicircularis and other slender slips are occasionally found. The nerves associated with the transverse abdominus are the intercostal, iliohypogastric, and the ilioinguinal.
NEUROANATOMY
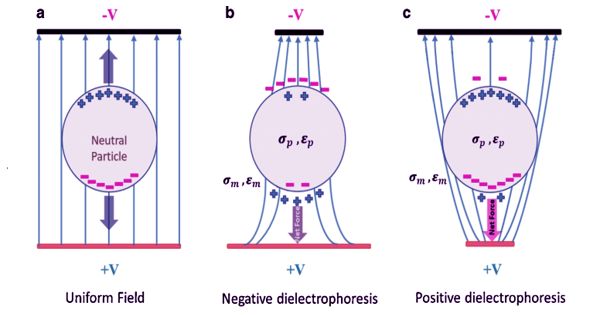
Neuronal innervations of the lower urinary tract is considered part of the autonomic and somatic nervous systems. The autonomic system (ie, the parasympathetic and sympathetic components) receives visceral sensation and regulates smooth muscle actively during conscious and involuntary lower urinary tract functions.
The autonomic nervous system constitutes the bulk of neural control of the lower urinary tract. Sympathetic contributions from T1-L2 and parasympathetic contributions from S2-4 compose the neuronal control system. Voluntary control of micturition is controlled by the central nervous system. Cortical control of the detrusor muscle rests in the supramedial portion of the frontal lobes and in the genu of the corpus callosum. Receiving both sensory afferent and modulating motor efferent nerves, the net effect is that the brain provides tonic inhibition of detrusor contraction.
Lesions in the frontal lobe chiefly cause loss of voluntary control of micturition and thus loss of suppression of the detrusor reflex, resulting in uncontrolled voiding or urge urinary incontinence. The pons and mesencephalic reticular formation in the brainstem constitute the micturition center. A reflex activation in the central brainstem and peripheral spinal cord mediate a coordinated series of events, consisting of relaxation of the striated urethral musculature and detrusor contraction that result in opening of the bladder neck and urethra. Lesions that interrupt these pathways have various effects depending on the level of interruption, essentially resulting in dyscoordination or dyssynergia of detrusor function.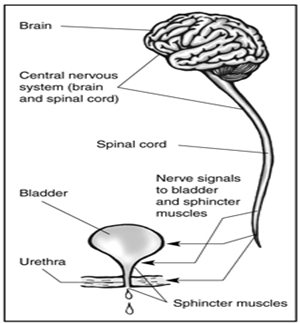
NERVES CARRY SIGNALS FROM THE BRAIN TO THE BLADDER AND SPHINCTER. ANY DISEASE, CONDITION, OR INJURY THAT DAMAGES NERVES CAN LEAD TO URINATION PROBLEMS
Innervation of the lower urinary tract is complex. Tight junctions between bladder smooth muscle cells allow for transmission of nerve impulses from cell to cell. The hypogastric nerve, originating from spinal cord segments of L1 through L4, supplies sympathetic innervation to the bladder and urethra. The pelvic nerve, originating from the spinal cord segments S1 through S3, supplies parasympathetic (cholinergic) innervation to the detrusor muscle and transmits sensory impulses from the bladder. Somatic innervation of the muscle of the external urethral sphincter is distributed via the pudendal nerve, originating from spinal cord segments S1 through S3. The pudendal nerve also innervates muscles of the anal sphincter and perineal region.
The storage phase of micturition is primarily controlled by the sympathetic and somatic nervous systems. Sympathetic stimulation of beta receptors in the detrusor muscle results in bladder relaxation to allow the bladder to fill. Sympathetic stimulation of alpha receptors in the neck of the bladder and internal urethral sphincter maintains continence. Sympathetic pathways also inhibit parasympathetic bladder innervation during storage. Stimulation of the pudendal nerve results in increased tone of the external urethral sphincter, contributing to continence. When the bladder is filled with urine, sensation is transmitted via the pelvic nerve to the sacral spinal cord, and subsequently to the brainstem. Voluntary control of urination originates from the cerebral cortex.
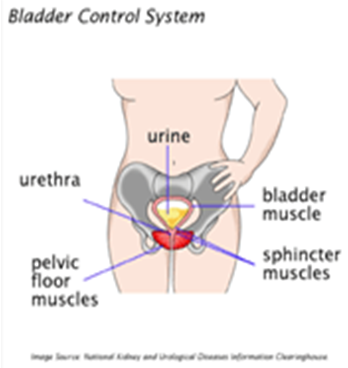
BLADDER CONTROL SYSTEM:
During the emptying phase of micturition, parasympathetic (cholinergic) stimulation of the detrusor muscle results in bladder contraction. Inhibition of sympathetic and somatic stimulation of the urethral smooth and skeletal muscle results in urethral relaxation. Following complete emptying of the bladder or voluntary cessation of urination, the storage phase begins again. External urethral sphincter tone can increase in response to sudden increases in abdominal pressure (during coughing or barking) to maintain continence.
Disruption of tight junctions between cells, peripheral nerves, spinal cord segments, or higher brain centers may alter micturition.
One of the major functions of the Urinary system is the process of excretion. Excretion is the process of eliminating, from an organism, waste products of metabolism and other materials that are of no use.
The urinary system maintains an appropriate fluid volume by regulating the amount of water that is excreted in the urine. Other aspects of its function include regulating the concentrations of various electrolytes in the body fluids and maintaining normal pH of the blood. Several body organs carry out excretion, but the kidneys are the most important excretory organ. The primary function of the kidneys are to maintain a stable internal environment (homeostasis) for optimal cell and tissue metabolism. They do this by separating urea, mineral salts, toxins, and other waste products from the blood. They also do the job of conserving water, salts, and electrolytes. At least one kidney must function properly for life to be maintained.
To maintain urinary continence, the ureters must empty into the urinary bladder in the correct location, the bladder must expand to accommodate increasing volumes of urine, and the urethra must exert tone greater than the resting pressure within the bladder and neurologic pathways to and from the bladder and urethra must be intact. For normal urination to occur, the bladder must be able to contract, contraction must be coordinated with urethral sphincter relaxation, and neurologic pathways must be intact.
The urinary bladder is composed of smooth muscle collectively referred to as the detrusor muscle. Smooth muscle of the urethra is contiguous with the detrusor muscle and is referred to as the internal urethral sphincter, although it is not a true anatomic sphincter. Skeletal muscle surrounding the urethra is called the external urethral sphincter.
Some are parts:
Training Isolated Kegels Exercise in Stress Urinary Incontinence (Part 1)
Training Isolated Kegels Exercise in Stress Urinary Incontinence (Part 2)