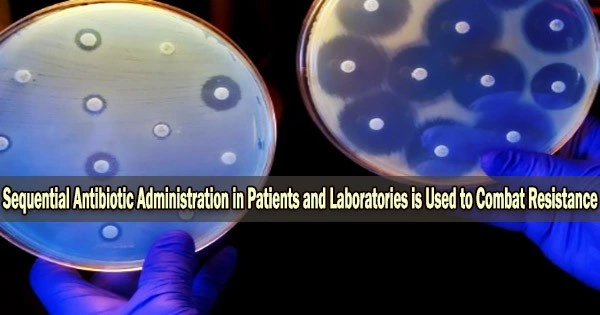
Recent findings from the Max-Planck-Institute (MPI) for Evolutionary Biology in Plön (Germany) reveal that quick antibiotic switching during a patient’s therapy may be able to successfully halt the emergence of resistance.
However, a number of variables affect how quickly the medications should be switched. One of these is, for instance, how the various medications interact.
Laboratory tests demonstrate that switching between medicines quickly helps stop the emergence of resistance. Collaterally sensitive drug pairings may be especially well suited for these treatments.
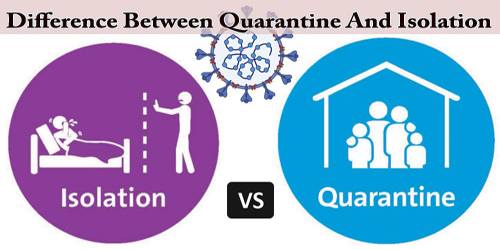
This implies that the bacteria become more susceptible to the other medicine as a result of drug resistance to one. The environment in which the bacteria in the patient live, however, is obviously different from that in a laboratory.
A significant distinction is that whereas medications can be swapped rapidly in the lab, in patients, natural degradation mechanisms cause antibiotic concentrations to fluctuate. In some periods, the doses of successive medication administrations may overlap. Drug interactions may affect the evolutionary dynamics during these moments of overlap.
Two comparative models
Doctoral researcher Christin Nyhoegen and research group leader Dr. Hildegard Uecker of the Stochastic Evolutionary Dynamics research group at the MPI in Plön created two mathematical models for comparison: a “laboratory model” and a pharmacokinetic-pharmacodynamic “patient model” to bridge the gap between the laboratory and potential clinical applications.
Our results show that sequential therapy might work well not only in the laboratory but also in the patient. However, the optimal strategy may vary slightly.
Christin Nyhoegen
The research shows that the bacterial population is consistently suppressed at least as well by treatments that switch pharmaceuticals more gradually as those that do so after each delivery.
Even though this is frequently the case while treating patients, sometimes switching slightly more slowly might be advantageous. This is particularly true when the medications interact negatively or the pharmacodynamic curve is steep and the germs multiply slowly.
“Our results show that sequential therapy might work well not only in the laboratory but also in the patient. However, the optimal strategy may vary slightly,” says Christin Nyhoegen.
Application in practice
Collateral sensitivity does not significantly benefit patients when there is no resistance present prior to therapy unless the cell division rate is modest and the medications are switched slowly.
In contrast, the effectiveness of treatments involving frequent drug switches is significantly impacted by drug-drug interactions. This demonstrates how crucial interactions may be for the best medicine pairing decision.
The findings are published in the Journal of The Royal Society Interface.
Initial attempts are being made to gather evidence of the efficacy of sequential therapy in patients using observational research, independent of the theoretical study. Results from both of these studies, as well as the theoretical one, can be used to develop randomized clinical trials, which are currently not feasible.