A review and analysis of data from 1,375 patients who underwent surgery to remove cancer from the kidney and inferior vena cava found that robotic surgery performed better than standard surgery. The inferior vena cava (IVC), the largest vein in the body, transports blood from the kidneys to the heart. Cancer can enter this vein and spread to the liver and heart. When compared to standard, open IVC thrombectomy, robotic IVC thrombectomy resulted in fewer blood transfusions and fewer complications overall in patients. The findings should prompt more research into the advantages of robotic IVC thrombectomy.
Kidney cancer does not always affect only one kidney. In advanced cases, cancer spreads to the body’s largest vein, the inferior vena cava (IVC), which transports blood from the kidneys to the heart. Cancer can spread to the liver and heart through the IVC. The Mays Cancer Center at The University of Texas Health Science Center at San Antonio (UT Health San Antonio) is one of the country’s busiest centers for treating this serious condition. San Antonio’s National Cancer Institute-designated Cancer Center is the Mays Cancer Center.
In a study featured on the cover of the Journal of Urology (Official Journal of the American Urological Association), researchers from the Mays Cancer Center and Department of Urology at UT Health San Antonio show that robotic IVC thrombectomy (removal of cancer from the inferior vena cava) is not inferior to standard open IVC thrombectomy and is a highly safe and effective alternative approach. The affected kidney is removed along with the tumor during surgery, which is performed at UT Health San Antonio’s clinical partner, University Hospital.
Open surgery has an excellent success rate, and it is used in the majority of cases. However, we can now achieve similar results with smaller incisions thanks to the robotic approach. As a result, we must investigate the implications of employing this newer approach.
Dharam Kaushik
Harshit Garg, MD, urologic oncology fellow in the Department of Urology, is first author of the study, and Dharam Kaushik, MD, urologic oncology fellowship program director, is the senior author. Kaushik is an associate professor and the Stanley and Sandra Rosenberg Endowed Chair in Urologic Research at UT Health San Antonio.
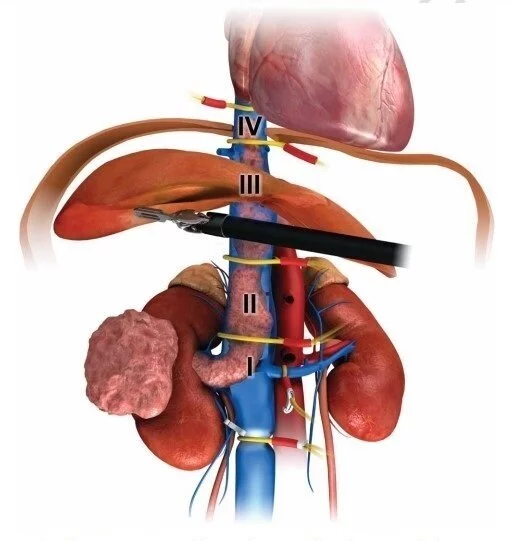
An incision 2 inches below the ribcage and extending downward on both sides of the ribcage is required for open surgery. “It appears to be an inverted V,” Kaushik said. Following that, the IVC’s surrounding organs, such as the liver, are mobilized, and the IVC is clamped above and below cancer. Surgeons gain control of the inferior vena cava in this manner, allowing them to perform cancer resection.
“Open surgery has an excellent success rate, and it is used in the majority of cases,” Kaushik said. “However, we can now achieve similar results with smaller incisions thanks to the robotic approach. As a result, we must investigate the implications of employing this newer approach.”
The study is a meta-analysis of data from 28 studies that enrolled 1,375 patients at various medical centers. 439 of these patients underwent robotic IVC thrombectomy, while 936 underwent open surgery. This study was carried out in collaboration with Memorial Sloan Kettering Cancer Center in New York, Cedars-Sinai Medical Center in Los Angeles, and the University of Washington in Seattle.
“We gathered the data to draw conclusions because, prior to this, only small studies from single institutions had been conducted to compare the IVC thrombectomy approaches,” Kaushik explained.
Findings
The results are encouraging and indicate further study of robotic IVC thrombectomy is warranted. The robotic approach in comparison with open was associated with:
- Fewer blood transfusions: 18% of robotic patients required transfusions compared to 64% of open patients.
- Fewer complications: 5% of robotic patients experienced complications such as bleeding compared to 36.7% of open thrombectomy patients.
These large, technically challenging surgeries last eight to 10 hours and involve a multidisciplinary team of vascular surgeons, cardiac surgeons, transplant surgeons, and urologic oncology surgeons, Kaushik said.
“This is the largest meta-analysis comparing the outcomes of robotic versus open IVC thrombectomy,” Kaushik said. “In over 1,300 patients, we discovered that the robotic approach reduced overall complications and reduced the need for blood transfusions.”
“That tells us there is more room for us to grow and refine this robotic procedure and offer it to patients who are ideal candidates for it,” Kaushik said. “Optimal candidacy for a robotic surgery should be based on a surgeon’s robotic expertise, the extent and burden of the tumor, and the patient’s comorbid conditions.” The open surgical approach remains the gold standard for achieving excellent surgical control.”