New research establishes a stronger link between fat and dementia. According to a study conducted by The University of Texas Health Science Center at San Antonio (UT Health San Antonio), higher levels of leptin, a hormone that aids in the maintenance of normal body weight, are linked to improved signal-transmitting brain white matter in middle-aged adults.
“The findings support the known role of leptin variations in late-life dementia risk by relating its deficiency with changes in white matter structure, which is an early event in the process of cognitive impairment due to Alzheimer’s disease or vascular dementia,” said Claudia Satizabal, PhD, associate professor at the Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases at UT Health San Antonio.
Satizabal is lead author of the study titled, “Leptin bioavailability and markers of brain atrophy and vascular injury in the middle age,” published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. Other authors also are with the Biggs Institute, as well as Tufts Medical Center in Boston; the Framingham Heart Study; Boston University School of Public Health; University of California-Davis; National and Kapodistrian University of Athens; and Columbia University.
The findings support the known role of leptin variations in late-life dementia risk by relating its deficiency with changes in white matter structure, which is an early event in the process of cognitive impairment due to Alzheimer’s disease or vascular dementia.
Claudia Satizabal
Obesity and Alzheimer’s
Alzheimer’s disease is the major cause of dementia, affecting millions of individuals around the world, according to the study. Increasing data suggests that midlife obesity contributes significantly to the chance of getting the condition.
This has sparked a rising interest in unraveling the processes linking obesity and Alzheimer’s, which may involve vascular, genetic, and metabolic pathways. And research into adipose or fatty tissue has shown considerable results.
Adipose tissue was once thought to be a passive reservoir for energy storage, but it is now considered a part of the endocrine system, secreting a group of bioactive peptides known as adipokines, or cell-signaling molecules that play functional roles in the body’s energy or metabolic status, inflammation, and obesity.
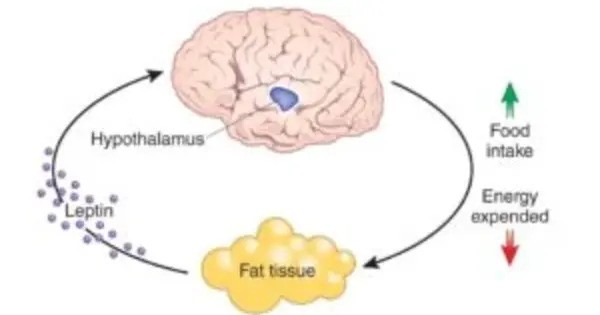
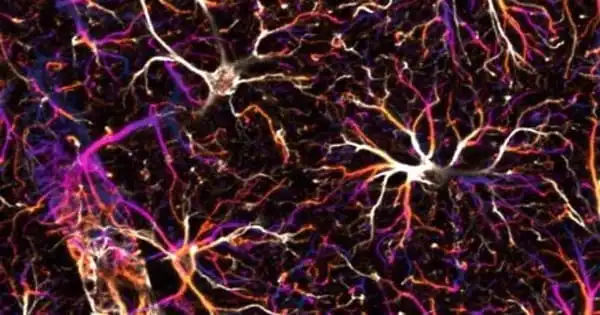
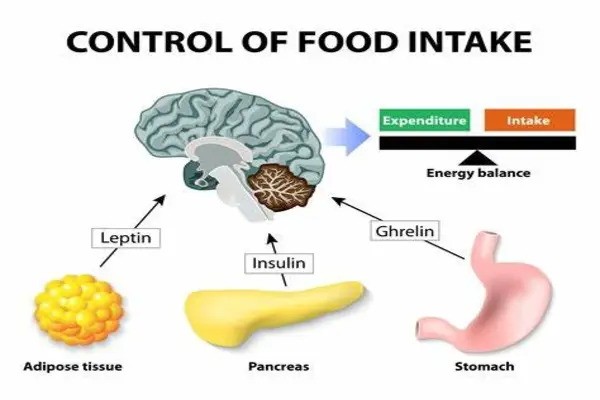
Leptin is an adipokine responsible for central control of food intake and energy homeostasis, and has been implicated in a variety of neurophysiological functions, including brain development, neurogenesis and neuroprotection.
Because of these effects, it has been considered a plausible mechanism in the pathway leading from obesity to Alzheimer’s disease. It is supported by findings tying higher leptin levels to lower risk for incident Alzheimer’s disease and mild cognitive impairment, as well as better structural brain indicators in older adults, the study notes.
Still, studies conducted in younger individuals have not detected associations between leptin and early indicators of brain damage preceding late-life dementia risk. Researchers in the new study at UT Health San Antonio aimed to gain further insights into the potential relationships of leptin with neurodegenerative and cerebrovascular burden.
Specifically, they investigated the associations of leptin markers with cognitive function and magnetic resonance imaging (MRI) measures of brain atrophy and vascular injury in healthy middle-aged adults.
They conducted neuropsychological evaluations of 2,262 cognitively healthy participants from the Framingham Heart Study, a long-term cardiovascular cohort study of residents from Framingham, Massachusetts, spanning three generations and now a project of the National Heart, Lung and Blood Institute, in collaboration with Boston University.
The researchers used enzyme-linked immunosorbent assays to evaluate the amounts of leptin, its soluble leptin receptor, and their ratio, known as the free leptin index, which indicates leptin bioavailability. Standardized techniques were used to obtain cognitive and MRI measurements.
The study discovered a stronger correlation between the soluble leptin receptor and reduced fractional anisotropy, a biomarker of brain white matter integrity, and peak-width skeletonized mean diffusivity, an imaging diagnostic for white matter injury. Similarly, a greater free leptin index was linked to higher fractional anisotropy.
These findings were replicated in a study involving 89 cognitively healthy Hispanic participants from San Antonio by MarkVCID, a consortium of academic medical centers in the United States whose mission is to identify and validate biomarkers for small vessel diseases of the brain that cause vascular contributions to cognitive impairment and dementia.
Overall, the researchers concluded that higher leptin bioavailability was related with superior white matter integrity in healthy middle-aged adults, indicating leptin’s potential neuroprotective function in late-life dementia risk.