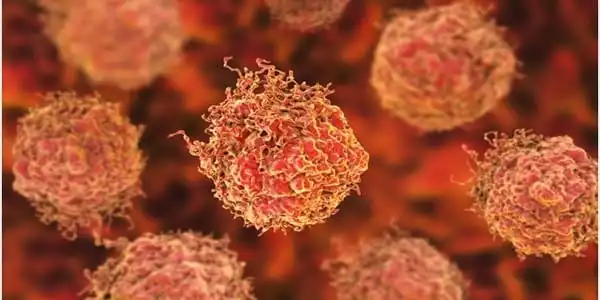
With the development of a new treatment that zeroes in on cancer cells to destroy them, prostate cancer treatment is on the verge of a major breakthrough. The therapy, known as 177Lu-PSMA-617, employs a molecule that seeks out and binds to a specific protein on the cancer cell surface. The radiation is then delivered by the technology, which damages the DNA and destroys the cancer cell. This treatment can locate and destroy cancer cells that have become resistant to other treatments.
Monash University researchers have established one of the world’s largest collections of living tumors from prostate cancer patients, accelerating the testing of new prostate cancer treatments and resulting in faster patient benefit.
Prostate cancer is one of the most common cancers, but it is also one of the most difficult to study in the laboratory, with the most commonly used models developed more than 40 years ago. With the formation of the Melbourne Urological Research Alliance (MURAL), hundreds of Victorian men generously donated samples of their cancer tissue, allowing the team to study a wider range of live tumors and test the efficacy of a wider range of therapies for their ability to stop tumor growth.
While the 10-year survival rate for men diagnosed with prostate cancer in the United States is around 98 percent, many men face difficult treatment decisions. They are concerned not only about which treatment will be most effective in fighting their cancer but also about how treatment will affect their quality of life.
Researchers have established one of the world’s largest collections of living tumors from prostate cancer patients, accelerating the testing of new treatments for prostate cancer and leading to faster patient benefit.
In general, advances in prostate cancer treatment over the last 10 to 15 years may have improved patients’ quality of life by lessening the severity of treatment side effects. They may also provide more specific information about a patient’s cancer stage and/or risk factors, which can help guide treatment decisions.
The PDX (patient-derived xenografts) collection, developed by a multidisciplinary consortium led by Professor Gail Risbridger and Associate Professor Renea Taylor at the Monash Biomedicine Discovery Institute (BDI), now includes 59 tumors collected from 30 patients between 2012 and 2020, making it one of the world’s largest collections of prostate cancer models.
Full characterization of the PDX collection is published in Nature Communications.
Researchers at the NCI are using magnetic resonance imaging (MRI) of the prostate in high-risk men to learn more about how frequently and how early these cancers occur. They’re also looking into whether regular scans in these men can detect cancers early before they spread to other parts of the body (metastasize).
MURAL PDXs are a long-term source of new cancer models that can be shared with other academic researchers or pharmaceutical companies. The patients and their families are directly involved in this venture, as is the EJ Whitten Foundation, which has been instrumental in providing over $1 million in donations over the last ten years, allowing this resource to be developed and the program to rise to the top of the international field.
“Patients like EJ Whitten are at the heart of this project from start to finish. We take patient tissue, test it in the laboratory, and the results advance patient treatment “Professor Risbridger stated. “Our new prostate cancer models have piqued the interest of scientists and the pharmaceutical industry all over the world.”
Ted Whitten, Executive Director and Founder of the E.J.Whitten Foundation, congratulates the Monash University Biomedicine Discovery Institute on its recent Prostate Cancer research findings. “We believe Monash University is a leader in prostate cancer research, and we have been thrilled to be able to financially support many of their important programs over the last ten years.”
“This resource provides an opportunity to link the molecular changes in prostate cancer to pathology, grow organoids, and test functional responses to therapies, which have rarely been applied to prostate cancer due to the lack of suitable models,” says Dr. Mitchell Lawrence, also from Monash BDI and a senior author.
This program’s success is based on collaboration between scientists and clinicians, such as Monash surgeons and oncologists, Cabrini Institute, and Peter MacCallum Cancer Centre, as well as patients and their families who generously donate cancer tissues. The Victorian Cancer Agency, the Prostate Cancer Foundation of Australia, and Movember are among the other organizations that contributed to the PDX program.