Antifungal drugs aren’t very effective right now. The problem is becoming increasingly difficult as these creatures, like bacteria, gain resistance to antimicrobial treatments.
Antibiotic resistance can occur in fungus, just as it can in bacteria when bacteria and fungi gain the ability to resist medications targeted to kill them. When fungus no longer responds to antifungal treatments, this is known as antifungal resistance.
Researchers report in the American Journal of Infectious Diseases that they have discovered chemicals that target these diseases in a novel way by interfering with fungal enzymes involved in the fatty acid synthesis, potentially paving the path for more effective treatments. Some fungi are naturally resistant to certain antifungal medications.
Invasive infections by Candida or other types of fungi can cause debilitating and deadly diseases like cryptococcal meningitis and some hospital-acquired infections, but superficial infections by Candida or other types of fungi can cause irritating but relatively minor conditions like oral thrush and athlete’s foot.
Antibiotics that include antifungal medications have been linked to antifungal resistance in Candida, according to certain research. This resistance could manifest itself in a number of ways.
Antibiotics, for example, can suppress both healthy and bad bacteria in the gut, allowing Candida to thrive. Although it is unclear if reducing the use of all or specific antibiotics can reduce Candida infections, proper antibiotic and antifungal drug use is one of the most critical aspects in combating drug resistance.
Researchers report that they have discovered chemicals that target these diseases in a novel way by interfering with fungal enzymes involved in the fatty acid synthesis, potentially paving the path for more effective treatments.
American Journal of Infectious Diseases
Because of the increased use of invasive surgery, implanted catheters, and immunosuppressive medication, more people are contracting these infections. Patients with severe COVID-19 or HIV, for example, are more vulnerable to fungal infections.
Treatments can also be hazardous, and they don’t always work, thanks to rising resistance. Molecules required for the formation of fungal cell walls are among the chemicals’ current targets.
As an alternative, Glen. E. Palmer and colleagues began researching prospective medicines that would function through a different mechanism and so avoid the downsides of these drugs.
Fungal fatty acid (FA) synthase and desaturase enzymes are critical for the proliferation and pathogenicity of human fungal infections, according to researchers. It’s been challenging to come up with a quick chemical assay to locate inhibitors for these enzymes because they’re tough to isolate.
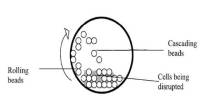
To screen thousands of tiny compounds, the scientists used a combination of genetic engineering and a whole-cell test. Although none of the substances examined decreased FA synthase activity in Candida albicans cell cultures, 16 of them did.
A core acyl hydrazide structure was discovered to be critical to the activity of several of these compounds, which were effective even against drug-resistant strains of several pathogenic fungi while causing little or no damage in mammalian cells. These chemicals, according to the researchers, are intriguing leads for further development as antifungal medicines.