A study team developed an early-stage therapy that sabotages the pump and restores antibiotic efficiency by disclosing the structure of a protein needed by bacteria to pump out antibiotics.
The new study, led by researchers from New York University, NYU Grossman School of Medicine, and NYU Langone’s Laura and Isaac Perlmutter Cancer Center, used advanced microscopy to “see” for the first time the structure of NorA, a protein that Staphylococcus aureus uses to pump out commonly used antibiotics before they can kill them.
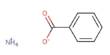
Efflux pumps are one method through which S. aureus has developed resistance to fluoroquinolone antibiotics, which include norfloxacin (Noroxin), levofloxacin (Levaquin), and ciprofloxacin (Cipro).
According to the researchers, fluoroquinolones are no longer effective against some drug-resistant bacterial strains, such as methicillin-resistant S. aureus (MRSA), which is a leading cause of death among hospitalized patients when infections become severe. As a result, researchers have been working to develop efflux pump inhibitors, although early attempts have been hampered by side effects.
“Instead of trying to find a new antibiotic, we hope to make the most widely used antibiotics over the last few decades, rendered ineffective by bacterial resistance, highly effective again,” says first study author Doug Brawley, PhD. He completed his doctoral thesis in the laboratories of senior authors Nate Traaseth, PhD, a professor in the Department of Chemistry at New York University, and Da-Neng Wang, PhD, a professor in the Department of Cell Biology at NYU Grossman School of Medicine.
Antibodies to the Rescue
The work, which was published online March 31 in the journal Nature Chemical Biology, relies on recent developments in antibody technology development. Invading bacteria cause the immune system to produce a variety of antibodies, which are proteins that are designed to adhere to and neutralize specific invaders.
Instead of trying to find a new antibiotic, we hope to make the most widely used antibiotics over the last few decades, rendered ineffective by bacterial resistance, highly effective again.
Doug Brawley
Antibodies were used in the current investigation to overcome a difficulty that had prevented the structure of NorA from being studied. Brawley spent years perfecting the expression and purification conditions for this study, but the NorA molecule is so small that even modern cryo-electron microscopy (cryo-EM) can’t detect it.
To locate the ones that linked the most tightly to NorA, the researchers examined a wide array of synthetic antibodies assembled by the lab of senior study author Shohei Koide, PhD, professor in the Department of Biochemistry and Molecular Pharmacology at NYU Grossman School of Medicine.
The team virtually doubled the size of NorA by attaching antibodies to it, which improved cryo-EM pictures and exposed the NorA pump’s structure for the first time. The research also revealed the location where the team’s lead antibody docked onto NorA, much like a key does in a lock.
The researchers were shocked to discover that the location where this antibody fit into NorA was the same location where NorA grabs onto medications and eliminates them. These findings suggested that the antibody could inhibit bacterial growth by blocking the pump and allowing antibiotics to remain inside bacterial cells.
The team also discovered that the region of the antibody most firmly lodged in NorA’s binding cavity was a short, looping peptide, a segment of protein building blocks, according to the cryo-EM structure.
“We became excited that an isolated peptide corresponding to the loop by itself might inhibit NorA,” says Traaseth.
When paired with the antibiotic norfloxacin, the scientists discovered that this peptide (termed NPI-1) functioned as an efflux pump inhibitor (EPI) and inhibited antibiotic-resistant S. aureus growth in dishes with nutrients (cultures) by more than 95% at high concentrations.
In the structural pocket where NorA connects to antibiotic molecules, the EPI had several interactions with protein building blocks, according to the structural study.
“This makes it highly unlikely that bacteria could develop resistance to such a treatment because they would have to randomly evolve to somehow defeat the EPI without taking away the ability of the efflux pump site to grab antibiotics,” says Wang.
The team is trying to improve the design of its EPI in the future. According to the authors, each NPI-1 residue can be adjusted for better efficacy and to reduce any potential negative effects.
Their approach to creating synthetic antibodies against NorA-like efflux pumps should aid in the discovery of EPIs for other diseases that rely on pumps, such as Streptococcus pneumoniae and Mycobacterium TB.
“The discovery of this new way to inhibit MRSA demonstrates that five labs from four departments with complementary expertise in structural biology, protein engineering, peptide chemistry, and microbiology can collaborate to accomplish what none could alone,” adds Koide.
Along with Brawley, Traaseth, Wang, and Koide, the authors of the study were David Sauer and Jinmei Song of the Department of Cell Biology; Jianping Li, Ganesh Jedhe, Tiffany Suwatthee, and Paramjit Arora of the Department of Chemistry; Xuhui Zheng and Victor Torres in the Department of Microbiology, Akiko Koide in the Department of Medicine, and Zheng Liu in the Cryo-Electron Microscopy Facility.
This work was supported by National Institutes of Health grants R01AI165782, R01AI108889, R01NS108151, R01GM121994, R01DK099023, R01AI099394, R01AI105129, R01AI137336, R01AI140754, R21AI149350, R35GM130333, and T32-GM088118; National Science Foundation award MCB 1506420; American Cancer Society Postdoctoral Fellowship 129844-PF-17-135-01-TBE, and Department of Defense Horizon Award W81XWH-16-1- 0153.
The research team also thanks NYU Grossman School of Medicine for its support in the cryo-EM Core facility, which was critical to the study’s findings.
The antibodies disclosed in this paper have been patented by New York University. Koide is a shareholder in Black Diamond Therapeutics and receives consulting fees from the company, as well as research funding from Puretech Health and Argenx BVBA.
Torres is a co-inventor on inventions and patent applications that NYU has submitted and that are currently licensed to Janssen Biotech Inc. These relationships are managed in accordance with NYU Langone Health’s regulations.