Okinawa Institute of Science and Technology Graduate University (OIST) researchers have discovered a protein that plays an important role in how the brain regulates appetite and metabolism. According to a new study published in the journal iScience, removing the protein XRN1 from the forebrain resulted in obese mice with an insatiable appetite.
Obesity is a growing public health concern, with over 650 million obese adults worldwide. Many diseases, including cardiovascular disease, type 2 diabetes, and cancer, have been linked to the condition.
“Fundamentally, obesity is caused by an imbalance between food intake and energy expenditure,” said Dr. Akiko Yanagiya, a researcher in Professor Tadashi Yamamoto’s Cell Signal Unit at OIST. “However, we still know very little about how communication between the brain and other parts of the body, such as the pancreas, liver, and adipose tissues, regulates appetite or metabolism.”
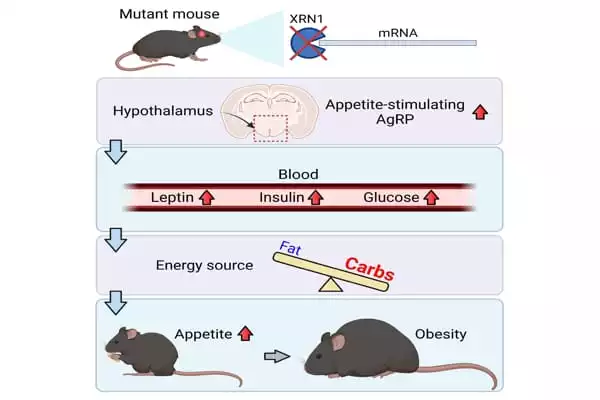
The researchers created mice that were unable to produce the protein XRN1 in a subset of forebrain neurons. The hypothalamus is an almond-sized structure in the brain that releases hormones into the body to help regulate body temperature, sleep, thirst, and hunger.
The scientists noticed that mice lacking XRN1 in the brain began to gain weight quickly at 6-weeks of age and became obese by 12 weeks of age. Fat accumulated throughout the mice’s bodies, including adipose tissue and the liver.
Fundamentally, obesity is caused by an imbalance between food intake and energy expenditure. However, we still know very little about how communication between the brain and other parts of the body, such as the pancreas, liver, and adipose tissues, regulates appetite or metabolism.
Dr. Akiko Yanagiya
When the researchers observed feeding behavior, they discovered that the mice lacking XRN1 ate nearly twice as much as the control mice. “This finding was really surprising,” said Dr. Shohei Takaoka, a former OIST Cell Signal Unit Ph.D. student. “We didn’t know what we’d find when we first knocked out XRN1 in the brain, but this drastic increase in appetite was very unexpected.”
To find out what was causing the mice to overeat, the researchers measured leptin levels in their blood, which is a hormone that suppresses hunger. The level of leptin in the blood was abnormally high in comparison to the controls, which would normally prevent the mice from feeling hungry. However, unlike the control mice, the mice lacking XRN1 did not respond to leptin, a condition known as leptin resistance.
The researchers also discovered that 5-week-old mice were resistant to insulin, a hormone released by beta cells in the pancreas in response to high blood glucose levels after eating. Failures in how the body responds to glucose and insulin can eventually lead to diabetes. The levels of glucose and insulin in the blood increased significantly as the mice aged, paralleling the rise in leptin levels.
“We believe that the rise in glucose and insulin levels was caused by a lack of response to leptin,” Dr. Yanagiya explained. “Leptin resistance meant that the mice continued to eat, keeping the blood glucose level high and, as a result, increasing insulin in the blood.”
The scientists then investigated whether the mice’s obesity was also caused by their use of less energy. They placed each mouse in a special cage that measured how much oxygen the mice used to calculate their metabolic rate indirectly.
The scientists found no overall difference in energy expenditure in mice aged 6 weeks. They did, however, discover something very surprising. The mice lacking XRN1 used carbohydrates as their primary energy source, whereas the control mice were able to switch between burning carbohydrates at night when they were most active, and fat during the day when they were less active.
“For some reason, this means that without XRN1, mice cannot effectively use fat as a fuel,” Dr. Yanagiya explained. “However, we still don’t know why this happens.” When the mice reached the age of 12 weeks, their energy expenditure decreased when compared to control mice. But, the scientists believed, this was an effect of obesity, due to the mice being less active, rather than a cause.
“Overall, we believe that overeating due to leptin resistance was the driving cause of these mice becoming obese,” Dr. Yanagiya said. To learn more about how XRN1 loss causes leptin resistance and increased appetite, the researchers examined whether the activity of appetite-regulating genes changed within the hypothalamus.
XRN1 is essential for gene activity because it is involved in the final step of messenger RNA degradation (mRNA). When a gene is activated, DNA is used to create a molecule of mRNA, which is then used to construct a specific protein. Cells regulate gene activity in a variety of ways, one of which is by degrading mRNA more slowly or quickly, resulting in more or less protein being produced, respectively.
The scientists discovered that in the hypothalamus, the mRNA used to make the protein Agouti-related peptide (AgRP) – one of the most potent appetite stimulators – was elevated in obese mice, resulting in higher levels of AgRP protein.
“It’s still just speculation, but we believe that an increase in this protein, as well as abnormal activation of the neuron that produces it, maybe the cause of leptin resistance in these mice,” Dr. Yanagiya said. “Leptin normally suppresses AgRP neuron activity, but if XRN1 is lost and this neuron remains highly active, it may override the leptin signal.”
However, the precise mechanism by which XRN1 loss leads to increased activation of AgRP neurons remains unknown. XRN1 was only removed from a subset of neurons in the forebrain, and AgRP neurons were not among them. This suggests that another neuron that did lose XRN1 may be involved, signaling incorrectly to the AgRP neurons and keeping them active.
Moving forward, the lab hopes to collaborate with neuroscience research units to determine exactly how XRN1 influences the activity of neurons in the hypothalamus to regulate appetite.