Scientists created eye tissue using patient stem cells and 3D bioprinting, which will help them understand the mechanisms of blinding diseases. The National Eye Institute (NEI), which is part of the National Institutes of Health, printed a mixture of cells that form the outer blood-retina barrier, which is eye tissue that supports the retina’s light-sensing photoreceptors. The technique allows researchers to study degenerative retinal diseases such as age-related macular degeneration with a theoretically infinite supply of patient-derived tissue (AMD).
“We know that AMD begins in the outer blood-retina barrier,” said Kapil Bharti, Ph.D., chair of the National Eye Institute’s Section on Ocular and Stem Cell Translational Research. “However, due to a lack of physiologically relevant human models, mechanisms of AMD initiation and progression to advanced dry and wet stages remain poorly understood.”
The outer blood-retina barrier is made up of the retinal pigment epithelium (RPE), which is separated from the blood-vessel-rich choriocapillaris by Bruch’s membrane. Bruch’s membrane regulates nutrient and waste exchange between the choriocapillaris and the RPE. Lipoprotein deposits known as drusen form outside Bruch’s membrane in AMD, impairing its function. The RPE degrades over time, resulting in photoreceptor degeneration and vision loss.
Our collaborative efforts have resulted in very relevant retina tissue models of degenerative eye diseases. Such tissue models have many potential uses in translational applications, including therapeutics development.
Marc Ferrer
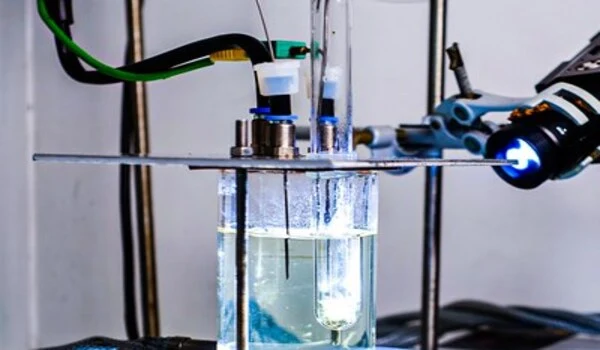
Bharti and colleagues combined three immature choroidal cell types in a hydrogel: pericytes and endothelial cells, which are key components of capillaries; and fibroblasts, which give tissues structure. The scientists then printed the gel on a biodegradable scaffold. Within days, the cells began to mature into a dense capillary network.
On day nine, the scientists seeded retinal pigment epithelial cells on the flip side of the scaffold. The printed tissue reached full maturity on day 42. Tissue analyses and genetic and functional testing showed that the printed tissue looked and behaved similarly to the native outer blood-retina barrier. Under induced stress, printed tissue exhibited patterns of early AMD such as drusen deposits underneath the RPE, and progression to late dry-stage AMD, where tissue degradation was observed.
Low oxygen-induced wet AMD-like appearance, with hyperproliferation of choroidal vessels that migrated into the sub-RPE zone. Anti-VEGF drugs, used to treat AMD suppressed this vessel overgrowth and migration and restored tissue morphology.
“By printing cells, we’re facilitating the exchange of cellular cues that are necessary for normal outer blood-retina barrier anatomy,” said Bharti. “For example, the presence of RPE cells induces gene expression changes in fibroblasts that contribute to the formation of Bruch’s membrane – something that was suggested many years ago but wasn’t proven until our model.”
Among the technical challenges that Bharti’s team addressed were generating a suitable biodegradable scaffold and achieving a consistent printing pattern through the development of a temperature-sensitive hydrogel that achieved distinct rows when cold but dissolved when the gel warmed. Good row consistency enabled a more precise system of quantifying tissue structures. They also optimized the cell mixture ratio of pericytes, endothelial cells, and fibroblasts.
Co-author Marc Ferrer, Ph.D., director of the 3D Tissue Bioprinting Laboratory at NIH’s National Center for Advancing Translational Sciences, and his team provided expertise for the fabrication of the outer blood-retina barrier tissues “in-a-well,” along with analytical measurements to enable drug screening.
“Our collaborative efforts have resulted in very relevant retina tissue models of degenerative eye diseases,” Ferrer said. “Such tissue models have many potential uses in translational applications, including therapeutics development.”