INTRODUCTION
The role of prenatal care is being increasingly questioned, particularly in resource poor environments in rural Bangladesh. The low predictability of prenatal markers for adverse maternal outcomes has led some to reject prenatal care as an efficient strategy in the fight against maternal and perinatal mortality. Few studies, however, have assessed the predictability of adverse outcomes other than dystocia or perinatal death, and most studies have been hospital based. This population-based cohort study was undertaken to assess whether prenatal screening can identify women at risk of severe labour or delivery complications in a rural area in Bangladesh. Antenatal risk markers, signs and symptoms were assessed for their association with severe maternal complications including dystocia, malpresentation, haemorrhage, hypertensive diseases, twin delivery and death. The results of the study suggest that antenatal screening by trained midwives fails to adequately distinguish women who will need special care during labour and delivery from those who will not need such care. The large majority of the women with dystocia or haemorrhage had no warning signs during pregnancy. A single blood pressure measurement and the assessment of fundal height, on the other hand, may detect a substantial number of women with hypertensive diseases and twin pregnancies. In addition, women who had an antenatal visit were four times more likely to deliver with a midwife than women who had no antenatal visit. Antenatal care may not be an efficient strategy to identify those most in need for obstetric service delivery, but if promoted in concurrence with effective emergency obstetric care, and delivered in skilled hands, it may become an effective instrument to facilitate better use of emergency obstetric care services.
Country`s health sector by now has accomplished many improvements and welcome changes for meeting health care needs of the people. Yet, it is painfully true that the reproductive role of women, particularly that of the rural women has remiend till now a high-risk area. The complications due to pregnancy and childbirth are still among the leading causes of mortality and morbidity of rural women. About 37-46 percent of all deaths and 17-35 percent of all sicknessess to the rural women of reproductive ages are due to them only (Koening M.A, et al.1988;Nahid , 1983;Begum,1996).And concern for women`s well-being, thus requires reproductive health of women to be taken seriously and accorded due priority.
Research on maternal health in Bangladesh is very scanty. A few studies available are confined primarily to maternal mortality(Chen et al,1974;Koenig et al,1988;Alauddin,1986;Khan et al;1986) The prenatal health, which is of great significance to women’s well-being recived little attention so far. Only study of worth mentioning in this regard has been conducted by the Bangladesh Institute of Research for Promotion of Essential and Reproductive Health and Teachnologies (Akhter H.H et al. 1996). This cross-sectional study has dealt with all kind of maternal morbility i.e. antepartum, intrapartum and postpartum, discussed certain risk factors of them and examined utilization of reproductive health care services by the women. While this is an elaborate study, its orientation has remaind more medical one is neglect of socioeconomic dimention of these health problems. Two other small studies mentioned these health problems of women (Islam and Hossain 1999;Ahmed et al, 1998).
The present paper is an attempt that information and it evolved around following themes:
- Extent of prenatal health risk of rural women and nature of these health problems.
- Association of select few socio-economic and demographic factors, such as women”s age, order of pregnancy, gestation womens education, household economic condition, and women’s employment status that are generally believed to affect the sociodemographic outcome in a society, with prenatal health risk of rural women;
- Extent and nature of antenatal care use by the rural women and influence of above mentioned socioeconomic and demographic variables on ANC utilization of them;and
- Current knowledge and practice of rural women regarding pregnancy and childbirth.
Prenatal fetus development
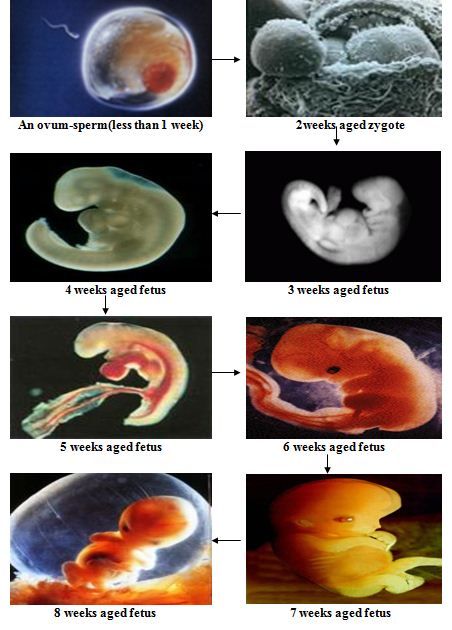
Pregnancy is typically broken into three periods or trimesters, each of about three months. While there are no hard and fast rules, these distinctions are useful in describing the changes that take place over time.
First trimester
Comparison of growth of the abdomen between 26 weeks and 40 weeks gestation.
Traditionally, doctors have measured pregnancy from a number of convenient points, including the day of last menstruation, ovulation, fertilization, implantation and chemical detection. In medicine, pregnancy is often defined as beginning when the developing embryo becomes implanted into the endometrial lining of a woman’s uterus. In some cases where complications may have arisen, the fertilized egg might implant itself in the fallopian tubes or the cervix, causing an ectopic pregnancy. Most pregnant women do not have any specific signs or symptoms of implantation, although it is not uncommon to experience light bleeding at implantation. Some women will also experience cramping during their first trimester. This is usually of no concern unless there is spotting or bleeding as well. The outer layers of the embryo grow and form a placenta, for the purpose of receiving essential nutrients through the uterine wall, or endometrium. The umbilical cord in a newborn child consists of the remnants of the connection to the placenta. The developing embryo undergoes tremendous growth and changes during the process of foetal development.
- Morning sickness can occur in about seventy percent of all pregnant women and typically improves after the first trimester.
- In the first 12 weeks of pregnancy the nipples and areolas darken due to a temporary increase in melanin.
- Most miscarriages occur during this period.
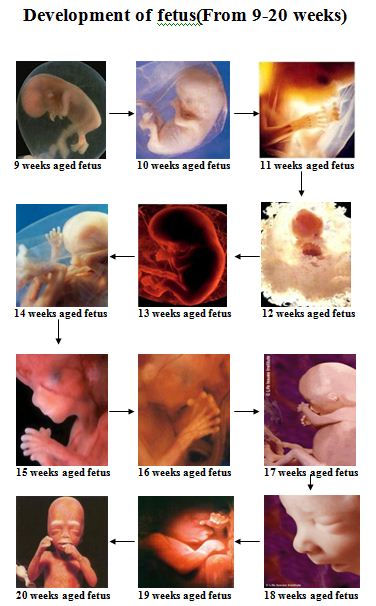
Second trimester
Months 4 through 6 of the pregnancy are called the second trimester. Most women feel more energized in this period, and begin to put on weight as the symptoms of morning sickness subside and eventually fade away.
In the 20th week the uterus, the muscular organ that holds the developing baby, can expand up to 20 times its normal size during pregnancy.
Although the fetus begins moving and takes a recognizable human shape during the first trimester, it is not until the second trimester that movement of the fetus, often referred to as “quickening”, can be felt. This typically happens in the fourth month more specifically in the 20 to 21 week or by the 18th week if you’ve been pregnant before. However, it is not uncommon for some women to not feel the baby move until much later. The placenta is now fully functioning and the fetus is making insulin and urinating. The reproductive organs can be recognized, and can distinguish the fetus as male or female.
Third trimester
Final weight gain takes place, which is the most weight gain throughout the pregnancy. The fetus will be growing the most rapidly during this stage, gaining up to 28g per day. The woman’s belly will transform in shape as the belly drops due the fetus turning in a downward position ready for birth. During the second trimester, the woman’s belly would have been very upright, whereas in the third trimester it will drop down quite low, the woman will be able to lift her belly up and down. The fetus begins to move regularly, and is felt by the woman. Fetal movement can become quite strong and be disruptive to the woman. The woman’s navel will sometimes become convex, “popping” out, due to her expanding abdomen. This period of her pregnancy can be uncomfortable, causing symptoms like weak bladder control and back-ache. Movement of the fetus becomes stronger and more frequent and via improved brain, eye, and muscle function the fetus is prepared for ex utero viability. The woman can feel the fetus “rolling” and it may cause pain or discomfort when it is near the woman’s ribs and spine.
It is during this time that a baby born prematurely may survive. The use of modern medical intensive care technology has greatly increased the probability of premature babies surviving, and has pushed back the boundary of viability to much earlier dates than would be possible without assistance. In spite of these developments, premature birth remains a major threat to the fetus, and may result in ill-health in later life, even if the baby survives.
Development of fetus(from 1-8 weeks)
Development of fetus(From 9-20 weeks)
DOCTORS PRESCRIPTION
1st trimester: Tab.Zn + Folic acid.
Tab. Bicarbonate.
Cap.Pentoprazole.
*Not: Never give Fe.
2nd trimester: Tab. Zn+ Folic acid + Fe + Bicarbonate.
Tab. Calcium + Vitamin D.
Tab. Pentoprazole
Inj. TT.
Last trimester: Tab. Zn + Folic acid+ Fe+ Bicarbonate
or Multivitamin.
Tab. Calcium + Vitamin-D.
Tab. Pantoprazole.
During pregnancy:
Anti-vomiting Drug.
Safest Antibiotics.
Drugs use in Pregnancy.
1.Azithromycin.
eg. Zimax. – Square.
Recent clinical studies have recommended that ‘Azithromycin’ should be considered for the initial treatment of chlamydial cervicitis in pregnancy.
2.Carbonyl iron, Zn Sulphate, Folic acid.
eg. Prenat-CI. – Healthcare Phamaceutical Ltd.
Function:
Carbonyl iron prevents:
- Severe anaemia.
- Birth and Maternal mortality
- Low birth weight.
Folic acid prevents:
- Neural tube defects.
- Habitual spontaneous abortion.
- Pregnancy complication.
3. Calcium and Vitamin-D 3 :
eg. IPICAL-D . – The IBN SINA Pharmaceutical Ltd.
It is highly effective in,
- Prevention of bone formation.
- Pregnancy induced hypertention.
- Bone and teeth formation of children.
- Proper hearing.
- Hip fracture reduction.
4. Domperidone.
eg. Ridone. – SK+F
This trial showed milk volume increased by 44.5% in the Domperidone group compared with 16% in the Placebo group.
5. Vitamin-E.
eg. Ovit-E. – Opsonin pharma.
Use in pregnancy and lactation in normal recommended dose.
6. Multivitamin and Multimineral.
eg. Precare. – Incepta Pharmaceutical Ltd.
Function:
- Vitamin-A: Development of embryo and healthy immune system.
- Vitamin-B1. Development of baby’s central nervous system and
- Vitamin-B2. Production of energy from food through metabolic
- Vitamin-B3. reaction.
- Vitamin-B5.
- Vitamin-B6.
- Folic acid. Synthesis of DNA and RNA and Maturation of RBC.
- Vitamin C. Development of healthy immune system.
- Vitamin E. Prevention of tissue damage through anti-oxidant action.
- Vitamin K. Helps in blood clotting so, prevent postpartum bleeding.
- Zinc. Healthy growth and development of baby.
- Iron. Formation of blood.
- Copper. Development of baby’s central nervous system and healthy
- Manganese. immune system.
- Iodine.
- Selenium.
- Molybdenum. Production of energy from food through metabolic reaction.
- Chromium. Stimulating the activities of enzyme.
- Inositol. Development of healthy immune system.
- Quercetin. Prevention of tissue damage through anti-oxidant action
and Improves lung function and reduces the risk of certain
respiratory disease, like asthma, bronchitis et
DATA.
The study utilized the information collected by a bigger study of BIDS ‘The Baseline Servey on Maternal and Neonatal Health Care in Selected Districts of Bangladesh’ (BIDS, 1996). The original study has collected information from several groups of women but present study utilized those collected from the pregnant women only. The study selected the sample pregnant women through several stages. First, four upazilas were selected from four pre-selected districts namely, Bhola, Feni, Tangail and Sirajganj on the basis of one Upazila from one districts using random procedure from the list of Upazilas two unions (Lowest administrative unit) were selected based on random principle. This produced eight unions from four districts. A house to house census with house hold head with the respondent was than conducted in all eight unions in order to locate pregnant women. These women were subsequently interviewed with a detail questionnaire and properly trained qualified women interviewer interviewed them in some privacy at home. All pregnancy related information presented in this study relates to their current pregnancy.
PROFILE OF SAMPLE PREGNANT WOMEN
Table 1 present few select background characteristics of the sample pregnant women. As shown by them, majority sample women are younger;19 percent of them is aged below 20 years and those aged between 20-24 represent 34 percent of them is aged above 35 years including 2 percent of them aged 40+
For 29 percent of them, the current pregnancy is the first order one, it is second order pregnancy for 23 percent and for 10 percent the current pregnancy is the fifth or higher order one. Majority sample women, thus are not only younger in age but biginners in reproductive carrer also. Indeed, given the fact that rural women complete most part of their reproduction by age 30-35 (DHS studies)and substantial decline has occurred in recent years in the higher order births of women above distribution of pregnancy order may be realistic.
Majority sample women , interestngly, has reported high gestation. Nearly half of them (48%) is in the third trimester (pregnant for 4-6 months), and 14 percent is in the first trimester (pregnant for 3 months or less). Although the distribution is highly skewed towards high gestation pregnancy this may reflect reality for seasonality of births recording a peak in December and January in the country (Becker and Sarder , 1978) and data being collected during September-December of the year. Nevertheless, one should bear in mind also that initial reporting about the presence of pregnant woman in the household was done by the household head who is often a male member in rural area. Thus, some pregnancies of initial stage disclosure of pregnancy at initial stage and few women may remain even unaware of them in early stage. In short, there are reasons for some omission to take place for early pregnancies.
Majority sample women are illiterate. Such women represent nearly two-third, 19 percent is educated up to primary level (grade 1-5), 12 percent up to secondary level (grade 6-10), and those with beyond secondary level education comprises of 4 percent. The matched figures for husband’s education are respectively 55, 21, 13 and 11 percent. Most of them (nearly two-third)belong to the poorer households with no or minimal landholding of less than half anacre. Only 10 percent of them belongs to households with more 2.50 acre of land and remaining 27 percent belongs to in-between land category (0.51 to 2.50 acres). The economically active women are few in numbers among them. Only 15 percent belong to this category and remaining 85 percent is housewife.
Distribution of Sample Pregnant Women by Socio-economic
and Demographic Characteristics
Socio-economic Characteristics | Percent women |
Age 15-19 20-24 25-29 30-34 35-39 40-44 45+ | 19.3 33.6 25.7 13.7 5.7 1.7 0.2 |
Order of pregnancy 0 1 2 3 4 5 6+ | 29.4 23.3 18.0 10.9 8.6 5.0 4.9 |
Education of husband Illiterate Primary Secondary Above secondary | 65.2 19.4 11.7 3.7 |
Education of women Illiterate Primary Secondary Above secondary |
54.9 20.8 13.1 11.2 |
Landholding size(in acres) <.50 .51-2.50 2.51+ |
63.4 26.8 9.7 |
Work Status Working Non-working | 15.2 84.8 |
Duration of Pregnancy(in month) <3 4-6 7+ | 14.0 38.2 47.7 |
Total | 2036 |
PRENATAL MORBIDITY
The prenatal morbidity discussed in this section refers to womens pregnancy related health problems. It does not include general health problems of them , such as those arise from diarrhoeal disease, respiratory problems, skin disease, gastricc/acidity, etc; although they too are able to affect the well-being of the mother.
Morbidity level:
The prenatal morbidity rates for the pregnant women referring to the ratio of pregnant women experienced some prenatal health problems to total pregnant women expressed in terms of 100, are presented in table 2. To note, those rates are being calculated from truncated observation viz., they have come from the pregnancies of incomplete term, hence, may underestimate the true rate for this morbidity. Underestimate of these rates also may arise due to socio-cultural reasons i.e. rural illiterate women may consider some such health problems, if not all, as the natural allies of pregnancy, thus, may refrain from reporting them.
Even this conservative estimates indicates that in rural area more than 60 percent (61 percent) of the women develop some maternal health problems during pregnancy. Age of them apparently has no influence on occurrence of this health risk but order of pregnancy seems to play some role. It has a J-shaped relationship with pregnancy related health risk suggesting high risk once at the beginning of reproduction and again at later stage. As observed it is high for the first order pregnancy, reduces for the second and third order ones, and increases again for 4th and higher order pregnancies. However, variation of this risk across pregnancy order does not seem to be marked one. The morbidity rate for the first order pregnancy is 62 percent, 57 percent for 3rd order ones, and around 64 percent for fifth and higher order pregnancies.
Gestation too has a J-shaped relationship with prenatal health risk but again of mild degree. The morbidity rate for first trimester pregnancy is 61.5 percent, 58 percent for trimester pregnancies. Above all what seems apparent from these statistics is that rural women start encountering maternal health problems soon after they conceive.
Percent of Pregnant Women Reported Pregnancy Related Health Problems
by Background Characteristics
Characteristic | Percent Women |
All | 60.8 |
Age of women <20 20-29 30-39 40+ | 61.2 59.8 64.0 59.0 |
Number of pregnancy 1 2 3 4 5+ | 62.2 58.8 56.7 62.3 63.9 |
Duration of pregnancy( in month) <3 4-6 7+ | 61.5 58.4 62.7 |
Education of women Illiterate Primary Secondary Above secondary | 59.0 65.0 62.2 68.4 |
Education of husband Illiterate Primary Secondary Above secondary | 59.4 63.1 58.6 66.4 |
Landholding (in acre) <.50 .51-2.50 2.51+ | 59.3 64.2 61.6 |
Work status Working Non working | 63.8 59.0 |
Socio-economic condition does not seem to have much influence on maternal health risk of rural women. No clear relationship is noted between such health risk and education of rural women and their husband although overall relationship tends to be a positive one. This may be due to better reporting of health problems by the rural educated women. The economic condition too has no notable influence on prenatal health risk of rural women but employment of them seems has some positive association viz., such risk is higher for rural working compared to those who do not work. The morbidity rate for the former is 64 percent and 59 percent for the latter.
Determinants of Prenatal Morbidity
Above observations with regard to the influence/association of select few socio-economic and demographic variables on prenatal health risk of rural women are obtained through bi-variate analysis of the data, hence, the observed relationship may not reflect the true relationship between them. For a clearer understanding of the situation, a multivariate analysis is carried out in this section. It is being done using Multiple Regression Techniqe (Morija,1990) but logistic form of it as the dependent variable of the analysis `the maternal health risk` is a binary variable. This variable has only two values i.e. either a women experienced a health problem or she has not for the current pregnancy. As expected, the analysis utilized various socio-economic and demographic factors discussed above as the independent or explanatory variables. All these variables except `womens work status’ are measured in interval scale. The work status of women being an ordinal variable is coded in the ‘dummy form’. A value of 1 is assigned to the ‘working’ status of women and zero to ‘non-working’ status; latter served as the ‘reference category’ (RC).
As shown by the analysis, controlling for the effects of other variables the net influence of none of the socioeconomic and demographic variables on prenatal health risk of rural women is significant at 5 percent level. Only two of them namely, duration of pregnancy and womens education came out significant at 10 percent level and both the variables showed a positive association with this particular health risk of women. These observations, however, require some explanations. As noted before, positive association between women’s education and prenatal health risk in the rural content may be an artifact of better reporting of health problems by the educated women. In case of gestation, such an association to an extent is in-built into the measurement of dependent variable ‘health risk’. This variable has a cumulative dimension viz., encountering health problems by the women cumulates over the gestation. Hence, we feel reluctant to put much emphasis on the observations made for them till further evidence is available.
As opposed to above, we are inclined to take note of the positive association noted between women’s work and their prenatal health risk despite it has failed to come out statistically significant. This is because results relating to them while have missed the significance level only by a small margin (Table 3) also require a larger gap between working and non-working women to be significant number of women being small (15 Percent ). The evident work effect also seems substantial. According to odds ratio, the odds of experiencing prenatal health problem by the rural working women is 23 percent higher than that of the rural non-working women.
In short, above analysis largely confirms the observations made through bivariate analysis that the prenatal health risk of rural women occurs primarily independent of socio-economic and demographic condition.
Nature of Prenatal Health Problems
Although a women can develop simultaneously several maternal health problems, only up to two of them is recorded. Distribution of them by nature of problem is presented in.
Note; Up to 2 health problems are recorded for a women.
1=Swelling in the leg; 2=Eclampsia /convulsion 3=High blood pressure
4=Anemia/malnutrition; 5=Abdominal pain 6=Vomiting/vomiting
7=Problems of heart; 8=Others tendency.
Three types of health problems ply the dominant role for prenatal morbidity of rural women. They are anemia/malnutrition, abdominal pain, and vomiting/vomiting tendency. Each of them accounts for about one quarter of the health problems reported by the pregnant women and the together, thus, account for nearly three-fourth of all pregnancy related health problems in rural area. Other important health problems are `swelling in the leg` accounting for 9 percent and convulsion, high pressure, problems relating to heart, headache, giddiness, bleeding, etc., give rise to another 15 percent.
According to prevalence rates, 22-23 percent women suffer from each of these three major health problems while 8 percent suffer from ‘swelling in the leg’ (table 5). Above figures rise to respectively 40 and 14 percent if estimates are kept confined to the sample women who experienced maternal health problems(table 5).
While above mentioned three major health problems ply the dominent role for maternal morbidity of the pregnant women in all socio-economic classes and across all demographic conditions, the elderly women aged above 30 and those in the advanced stage of pregnancy tend to suffer relatively more from anaemia/malnutrition. This may be due to cumulative effects of women’s reproductive role; both repeated pregnancy and pregnancy of higher gestation causing presumably through greater depletion of nutrition render rural women more vulnerable to malnutrition/ anaemia. Yet, an interesting observation is that prevalence of anaemia/malnutrition varies by a small degree only across socio-economic condition through the disadvantaged women tend to suffer more from it (table 5, upper panel). This may be related to pregnancy related peculiarities. The vomiting and vomiting tendency that the women develop during pregnancy presumably by disrupting food intake of all leads to this. Also, the cultural restriction of food during pregnancy may contribute towards it (Bhatia et ai. 1979). What then appears is that in rural area socio-economic condition play a restricted role for nutrition of pregnant women.
The abdominal pain is more common with the elderly women (aged above 30) and those in advanced stage of pregnancy. It varies little across socio-economic condition (table 5). Vomiting and vomiting tendency is more a problem of younger women (aged below 30) and its prevalence is noticeable high in initial stage of pregnancy. 43 of the total complains made by the first trimester pregnancy is vomiting only while corresponding figure among third trimester pregnancy in 18 percent. Interestingly, highly educated and better off women suffer more from vomiting than their counterparts who are poor and illiterate or semi-literate (Table 4 and 5). This may be due to perception variation about maternal health problems viz., educated and better-off women perhaps view them more as health problem, while latter consider them more as natural allies of pregnancy.
The ‘swelling in the leg’, on the other hand, is a problem of advanced stage of pregnancy only. Little more than 1 percent of the maternal health problems of the first trimester pregnancy represent this against 5 percent among third trimester pregnancies. Of total such problems reported by the sample pregnant women, three-fourth is made by the third trimester pregnancy alone.
As the above evidence, therefore, indicates, rural women not only face similar risk from prenatal morbidity but suffer also in general from similar kinds of health problems. socio-economic condition hardly involves any noticeable variation for these.
ANTENATAL CARE(ANC)
Antenatal care(ANC) is a package of services rendered to women during pregnancy with an aim to improving maternal mortality and morbidity. however, for achieving these objectives number and timing of ANC visit is important. Ideally, this care should begin soon after the conception takes place and continue throughout the pregnancy at regular interval. As recommended generally, ANC visit be made monthly for the first seven months, fortnightly in the eight month, and then weekly until the birth (Mitra et al., 1997). The ideal number of ANC visit throughout 40 weeks of pregnancy thus ends up to 12-14. In Bangladesh where access to and utilization of such care is very poor three minimum visits keeping the maximum number open to ideal number is recommended for ANC (Islam A, 1994); Family Planning Directorate/UNICEF, 1994).
Unfortunately, the present study has no information on timing of start of the ANC visit and on number of such visit made by the women. Also, no direct information on ANC use is known. Under this circumstance, identification of ANC use is approached indirectly. It is assumed that the sample pregnant women who reported some maternal morbidity and also some use of health care are thought to have received some pregnancy related care falling under the ambit of ANC. However, in all such cases visit to the provider may not have done in connection with maternal morbidity but for other health problems. But this again may not be fully correct, hence, the level of ANC use estimated in the study may represent an upper limit for this.
Level of ANC
Table 6 presents the proportion of sample pregnant women who utilized some such care. This figure is derived from two bases, one, relates to total pregnant women (Col.2) and other to the women women who reported some prenatal health problems (Col.3).
Percent of pregnant Women Received ANC by
Background Characteristics
| Characteristics | Of all pregnant Women | Of those Reported Health Problem(s) |
All | 29.4 | 48.3 |
Age <20 20-29 30+ | 31.0 27.9 31.8 |
50.2 46.7 50.5 |
Duration of pregnancy <3 months 4-6 7+ |
7.3 23.5 40.5 |
11.9 40.3 64.7 |
Education of Women No education Primary Secondary Above secondary |
26.0 33.8 34.9 48.7 |
44.0 51.9 45.3 100.0 |
Education of Husband No education Primary Secondary Above secondary |
26.0 30.0 32.7 40.6 |
43.8 47.6 37.3 100.0 |
Land size(in acre) <.50 .51-2.50 2.51+ |
26.3 34.7 34.3 |
44.4 54.1 55.7 |
Work Status Working Non-working |
32.7 28.8 |
51.2 48.8 |
Under above assumption it is being observed that 29 percent of the rural pregnant women receive some kind of prenatal health care. The figure rises to 48 percent for the women who encounter maternal health problems. Thus, not only more than 70 percent of the rural pregnant women are outside the purview of antenatal care but also more than half of the pregnant women do not seek any such care even when the suffer from felt maternal health problems.
Age of women matters little for utilization of ANC. The utilization rate of ANC is about similar over the ages. The gestation or duration of pregnancy apparently is positively associated with ANC utilization. The ANC utilization rate is 7 percent for the first trimester pregnancies and 41 percent for third trimester ones (Table 6, Col.2). However, as noted before for maternal morbidity, the ANC utilization too has a cumulative dimension over gestation. Such as association therefore, to an extent, is in-built between them. In reality, the may or may not have any such relationship.
Education of women and husband renders positive influence on ANC use although it is stronger in case of women’s education. Nearly half of the highly educated women (secondary and above) and 40 percent of the wives of highly educated men reported make use of this care against 26 percent dose so among uneducated class. Yet, one point to note is that even among highly educated rural women having beyond secondary level education more than half dose not seek any ANC. They, however, do not hesitate to seek this care when there is a problem although in such cases uneducated class only in 44 percent cases seeks ANC (Table 6, Col.3).
Economic condition too renders a positive influence on ANC utilization but this dose not seem to be strong one. The utilization rate for the poorer women is 26 percent and 34 percent for richer section (highest land owning class) (Table 6). The influence of women’s employment too is positive. The ANC utilization rate for working women is 33 percent and that for non-working women is 29 percent.
Determinants of ANC Use
Like that of maternal morbidity, above observations with regard to the influence of various socio-economic and demographic variables on ANC utilization are obtained through bi-variate analysis of the data. thus all of them may not reflect the true situation. As done before, for a clearer understanding of the phenomena a multivariate analysis is carried out in this section. The analysis is carried using the ‘ANC use’ as the dependent variable and socio-economic and demographic variables as the explanatory variables. The dependent variable ‘ANC use’ again is a binary variable having two values only i.e. a women either utilied ANC or not by the time of survey with former assigning a value of 1 and latter 0, hence, proposed analysis is conducted utilizing logistic form of the multiple regression technique. The explanatory variables are measured as before viz., all of them except for women’s work are measured in interval scale and ‘work status’ is coded in the dummy from with ‘work status’ assuming a value of 1 and ‘non-working’ status zero.
The regression results (Table 7) show that controlling the effect of other variables the net influence of women’s age and order of pregnancy on ANC utilization is almost absent. They matter hardly for this. Gestation has a significant positive influence. But as noted before, the relationship has an in-built component. We, therefore, prefer to ignore it.
Among socio-economic variables, the results are significant and positive for education only and it is so both for women and husband education. All other variables statistically insignificant. According to odds ratio, one year increase in women’s education increases the odds of ANC use by about 6 percent and that of husband’s education increases the same by about 4 percent (Table 7). What then emerges is that in rural area, only education has recognizable effect on ANC use. Others variables are yet to assume importance for this.
Effect of Socio-economic and Demographic Variables on ANC Use
| Variables | Odds Ratio | P-value |
Age of Women Order of Pregnancy Gestation Education of Women Education of Husband Land Employment | .9991 .949 1.472 1.058 1.036 1.006 1.169 | .9843 .1320 .0000 .0076 .0241 0.561 .2526 |
REPRODUCTIVE KNOWLEDGE AND PRACTICE
Rural women’s knowledge and practice with regard to maternity or pregnancy and child-birth are documented in this section. This is being done to gather some idea about the progress made so far towards the ‘safe motherhood’ practice, which holds the key to reducing reproductive risk for the women.
Knowledge
Table 8 presents the knowledge level of rural women with regarded to certain aspects of reproduction. The knowledge level apparently is found quite high on them. For example, more than 80 percent of them is aware of the need of sufficient quantity of food, adequate rate, avoidance of hard manual work, need for medical check-up and TT injection during pregnancy. The knowledge level is found highest for the TT injection and lowest for the monthly medical check-up. Almost all rural women (97 percent) currently know about TT injection and 80 is aware that the women should undergo monthly medical check-up during pregnancy. Other aspects are know by 92/93 percent of the rural women (Table 8).
Above observations indicating high knowledge level, however, are in contradiction with earlier findings that there exists widespread ignorance about maternity and maternal health among rural women. This anomaly tends to suggest that the knowledge level demonstrated above may be ‘mere knowledge’ only and not an effective knowledge of the women.
This conjecture has some support from the data. For example, although as many as 97 percent of the rural women know about TT injection and 85 percent of them have received it in reality, only 37 percent of them knows about the requirement of total 5 doses of TT injection during entire reproductive period (Table 9)
Food intake
Although more than 90 percent of the sample pregnant women is aware of the need for adequate quantity and quality of food during pregnancy actual practice of them is found different. Only less then 10 percent of them consume more than usual quantity and quality of food while another 5 percent consume some improved variety of food like egg, milk, meat, fruits, etc. Remaining 85 percent reported consumption of usual quantity/quality of food or less than that (Table 10). In view of the fact that nearly half of the country’s rural population live below the poverty line (Sen, 2001) this latter group representing 85 percent is likely to fell vulnerable to anaemia/malnutrition with a quarter consuming less than normal share encountering the risk of severe malnutrition. It is no wonder, therefore, that the anaemia/malnutrition is so prevalent among rural mothers giving rise to extraordinary high incidence of low birth weight babies
Women’s age appears to have some influence on food intake. Compared to older pregnant women food intake is better for younger ones. Only 10 percent among former consumes more than normal share of food against 20 percent for the latter. Perhaps, pregnancy being a new phenomenon for the latter receives an extra attention while it may be a routine affair with the former. The food intake of pregnant women is affected more at initial than later stage of pregnancy and this may be due to vomiting/vomiting tendency women develop in early stage
Improved socio-economic condition influences the food-intake positively but in case of education of such influence becomes visible only at higher level after secondary level. An interesting point to note is that roughly an equal proportion of women across all socio-economic classes consumes less than normal share of food during pregnancy. Again this may be a pregnancy-induced phenomenon and may be linked to the vomiting and vomiting tendency that the women generally develop during early stage of pregnancy. Hence, as it seems, socio-economic condition remains partly effective for food intake during pregnancy. Women’s employment is of no significance in this regard.
DISCUSSION & CONCLUSION
The field level evidence of our country clearly suggests that the reproductive health of women although features prominently in the government policy document the ground reality has been different. The maternal health risk for the rural women is still quite high with more than 60 percent of the pregnant women encountering maternal morbidity. Such high risk is not confined to any particular group of women. Rather, community, at large, susceptible to it.
Further depressing fact is that the access of rural women to the reproductive health care playing a crucial role in reducing the maternal mortality and morbidity is still highly inadequate. Only less one-third of the pregnant women currently use some antenatal care. Their access to other ‘safe delivery practices’ is also very limited suggesting no notable progress in this regard. Almost all rural women still prefer to deliver the child at home and 95 percent is assisted by friends, relatives, neighbors, local dai, etc., for the delivery. Hence, reproductive health of the women seems has remained as yet a rhetoric or a commitment in paper representing the weakest part of our health care system. It is, therefore, both urgent and necessary that the government undertakes its commitments in this regard with all seriousness for necessary improvement of women’s health.
For deriving best possible results, thrust, however has to be made to be improve the quality of the services along with proper packaging of it. Given the evidence, a first task in this regard would be to enlarge the present scope of ANC beyond TT injection to include other basic elements of the antenatal services. It should be desired such that along with management of the physical problems the risk pregnancies can be detected well in advance for precautionary measures.
The issue of women’s access to reproductive health care has to be addressed, however, both from supply and demand point of view. While there is known supply limitation of the services evidence also suggests that these services suffer from adequate demand also. Hence, along side the endeavors to mitigate supply side constraint efforts are to be made to create demand for them. Given the present evidence there persist widespread ignorance and lack of appreciation about maternity and maternal role in rural area putting severe restriction on the demand for these services. In addressing demand side problem, a necessary first step thus would be to put in place the appropriately designed Information Education and Motivation (IEM) program so that the rural women as well as the larger community become aware of the need of this care in view reproduction its right perspective. For a lasting and sustained effect, women’s agency role through education, however, has to be improved. Of all socio-economic variables, women’s education is found strongly and positively related to ANC utilization in rural area.
For vast number of rural women being outside the purview of ANC, delivering ANC services to the rural women may appear a challenging task. Yet, given the evidence that the system of delivering primary antenatal care to rural women through the field level health and family planning workers is working reasonably well, the task may be made easier. It is possible to increase rural coverage of these services through proper utilization of the workers. Also, Satellite Clinics fetching highest use from rural women can be arranged more frequently with priority ANC services to help this process.
Finally, the public sector has to play a dominant role in delivering reproductive health care services to the rural women who are mostly poor, less empowered, and deprived. The market-oriented health care system may not meet this special health care of rural women satisfactorily. Also, current bias of the MCH policy package towards contraception delivery and infant and child mortality requires modification to give due emphasis on women’s health for achieving better results.