The blood-brain barrier (BBB) is a network of specialized cells that line the blood vessels in the brain and prevent certain substances from entering the brain tissue. The BBB is an important defense mechanism that helps to maintain a stable environment in the brain and protect it from harmful substances.
A common symptom of COVID-19 is a partial or complete loss of smell. The virus is considered to affect the sensory neurons in the olfactory epithelium by infecting sustentacular cells in this epithelium.
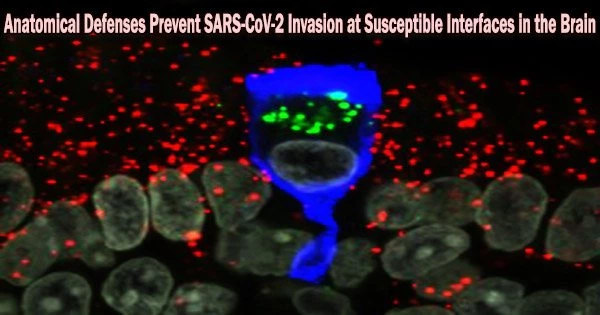
Scientists at the Max Planck Research Unit for Neurogenetics in Frankfurt in collaboration with physicians and scientists at the University Hospitals Leuven (Leuven, Belgium) and hospitals in Bruges and Brussels, Belgium, have now examined tissue samples of nasal mucosa and brain of patients who died from or with a SARS-CoV-2 infection, including the delta, omicron BA.1 or BA.2 variants.
The researchers looked at more over a hundred COVID-19 patients in all, but they couldn’t find any signs of viral invasion of the brain. One of numerous anatomical barriers that protect the brain from the virus at vulnerable interfaces appears to be a poorly understood class of fibroblasts in the olfactory mucosa.
After SARS-CoV-2 infection, anosmia which can range from a brief impairment to a persistent, potentially permanent loss of smell occurs often. One of the main entrance points for the virus is the nasal mucosa.
Early in the pandemic, there was concern that the virus would affect olfactory epithelial cells, travel through the olfactory nerve, and ultimately infect or enter the brain through the neighboring olfactory bulb, which is situated just a few millimeters from the nasal cavity.
But this suspicion has not been confirmed. In November 2021, scientists at the Max Planck Research Unit for Neurogenetics in Frankfurt, together with physicians and scientists in Leuven and Bruges, Belgium, reported that SARS-CoV-2 infects the sustentacular cells (supporting cells) of the olfactory epithelium, but not the sensory neurons. The researchers were unable to detect the virus in the olfactory bulb.
For the purpose of taking tissue samples from patients who had passed away, the doctors had created a bedside surgical technique. In a cohort of 70 COVID-19 patients, they were able to collect complete olfactory bulbs and tissue samples from the frontal lobe of the brain, respiratory mucosa, and olfactory mucosa within an hour or two of the moment of death using this novel method. The tissue samples are exceptionally well suited for molecular and histological research because of the unusually short postmortem period.
We examined microscopically the olfactory bulbs and the frontal lobe samples for viral nucleic acid and protein. All samples were negative: no neurons were infected. Moreover, by trying to culture SARS-CoV-2 from cerebrospinal fluid samples, we could not find evidence that SARS-CoV-2 had invaded the brain.
Peter Mombaerts
All brain samples were negative
Currently, the team is analyzing tissue samples from a second cohort of 45 COVID-19 patients who died within two weeks of their diagnosis and had either the delta, omicron BA.1 or BA.2 versions of the virus.
Additionally, they examined tissue samples from the frontal lobes of the brains of the majority of COVID-19 patients from the first cohort who had the alpha or non-variants of concern.
“We examined microscopically the olfactory bulbs and the frontal lobe samples for viral nucleic acid and protein. All samples were negative: no neurons were infected. Moreover, by trying to culture SARS-CoV-2 from cerebrospinal fluid samples, we could not find evidence that SARS-CoV-2 had invaded the brain,” says Peter Mombaerts of the Max Planck Research Unit for Neurogenetics.
Adds Laura Van Gerven, ENT surgeon at the University Hospitals Leuven, Belgium, “SARS-CoV-2 would have the greatest chance of displaying its hypothetical neurotropic or neuroinvasive capacity in these highly vulnerable patients, with a colossal failure of the host defense and the gravest outcome of all.”
The olfactory nerve’s thin, elongated cells known as perineurial fibroblasts, whose purpose is unknown, appear to serve as a protective anatomical barrier. They encircle the olfactory nerve bundles in one or more layers that are closely packed.
“We do not know how these cells prevent the virus from invading the olfactory nerve bundles. But they seem instrumental in preventing SARS-CoV-2 and possibly some of the many other pathogens that infect the nasal mucosa from invading the brain,” Mombaerts explains.
The paper is published in the journal Neuron. The hypothesis that SARS-CoV-2 invades the brain and infects brain cells is not supported by the latest findings. The conclusions have effects on lengthy COVID’s underlying mechanics.