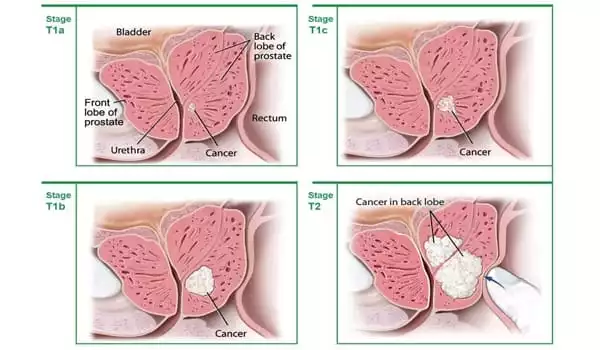
Screening with a prostate-specific antigen (PSA) test has been shown to reduce the number of deaths from prostate cancer. However, prostate cancer is frequently so slow-growing that it would not cause a man any problems during his lifetime. As a result, many men do not benefit from prostate cancer treatment and may unnecessarily suffer from its side effects, such as long-term urinary and sexual function problems.
Magnetic resonance imaging (MRI) could reduce overdiagnosis and thus improve prostate cancer screening, according to researchers at Sweden’s Karolinska Institutet. The same research team has now published a study in The Lancet Oncology demonstrating that the addition of a novel blood test, the Stockholm3 test, can reduce the number of MRIs performed by one-third while also preventing the detection of minor, low-risk tumors.
“Overall, our research indicates that we have identified the tools required to perform effective and safe prostate cancer screening. It feels fantastic to be able to present knowledge that can improve men’s healthcare after many years of debate and research “Tobias Nordström, associate professor of urology at Karolinska Institutet’s Department of Clinical Sciences, Danderyd Hospital, is in charge of the STHLM3MRI study.
Researchers recently reported that magnetic resonance imaging (MRI) could reduce overdiagnoses and thereby improve prostate cancer screening.
Current screening methods, which combine PSA (prostate-specific antigen) tests with traditional biopsies, result in unnecessary biopsies and the detection of a large number of minor, low-risk tumors (overdiagnosis). As a result, with the exception of Lithuania, no country has chosen to implement a nationwide prostate cancer screening program because the benefits outweigh the drawbacks.
“Prostate-specific antigen (PSA) screening for prostate cancer reduces mortality but can have negative consequences. We wanted to see how a traditional screening approach compared to a diagnostic strategy of blood-based risk prediction combined with MRI-targeted biopsies,” the researchers write.
“In Stockholm County, Sweden, we conducted a prospective, population-based, randomized, open-label, non-inferiority trial (STHLM3-MRI).” Statistics Sweden randomly selected men aged 50–74 years and mailed them an invitation to participate in screening; those with an elevated risk of prostate cancer, defined as a PSA of 3 ng/mL or higher or a Stockholm3 score of 0•11 or higher, were eligible for randomization.”
The STHLM3MRI study’s findings were published in The New England Journal of Medicine, indicating that replacing traditional prostate biopsies with magnetic resonance imaging (MRI) and targeted biopsies could reduce overdiagnosis. The new findings, published in The Lancet Oncology, show that the addition of the Stockholm3 test, developed by Karolinska Institutet researchers, can be a valuable supplement. It is a blood test that analyzes a combination of protein markers, genetic markers, and clinical data using an algorithm.
“The availability of MRI in healthcare will be a constraint. We now demonstrate that a novel blood test used in conjunction with MRI can reduce the number of MRIs performed by one-third. Overdiagnosis is reduced by up to 69 percent when compared to traditional screening. At the same time, the number of biopsies is cut in half, while the number of clinically significant tumors remains the same “Martin Eklund, associate professor at Karolinska Institutet’s Department of Medical Epidemiology and Biostatistics and co-author of the STHLM3MRI study, agrees.
STHLM3MRI is a randomized study with 12,750 male participants from Stockholm County that took place between 2018 and 2021. Participants provided an initial blood sample for PSA analysis as well as analysis with the new Stockholm3 test. Men with elevated PSA levels were then chosen at random for traditional biopsies or MRIs. Biopsies were only performed on suspected tumors identified by MRI in the MRI group.
“Using the Stockholm3 test and MRI separately has previously been shown to be cost-effective. We have now analyzed the cost-effectiveness of combining these tools and will soon report exciting results from that analysis “Tobias Nordström sums up.
Current screening methods used in conjunction with traditional biopsies result in unnecessary biopsies and the detection of many smaller, low-risk tumors. As a result, with the exception of Lithuania, no country has chosen to implement a national prostate cancer screening program because the benefits outweigh the drawbacks.