One of the leading causes of cancer-related deaths in men is prostate cancer (PC). Various aspects of cancer epigenetics are rapidly evolving, and the role of two major epigenetic changes in prostate cancer, including DNA methylation and histone modifications, is being extensively researched.
Scientists at the Garvan Institute of Medical Research have discovered new epigenetic biomarkers that can predict more aggressive forms of prostate cancer. The biomarkers, when combined with traditional clinical tools, can predict whether a man will develop a more metastatic and lethal form of the disease, potentially assisting clinicians in developing a better treatment plan.
“Men with prostate cancer need more personalised treatments guided by the nature of their tumors, and they can’t get that without new biomarkers that can better predict the risk of developing the lethal form of the disease,” says Professor Susan Clark, Head of the Epigenetic Research lab at Garvan and the study’s lead researcher.
Prostate cancer is the second most common cancer diagnosed in men worldwide. After being diagnosed, approximately half of all men will develop metastatic cancer during their lifetime. Metastasis typically takes 15 years or more to develop, but a small percentage of men develop a fatal, metastatic form much sooner after diagnosis.
Men with prostate cancer need more personalized treatments guided by the nature of their tumors, and they can’t get that without new biomarkers that can better predict the risk of developing the lethal form of the disease.
Professor Susan Clark
By identifying patients who might go on to develop this form of prostate cancer at the early stages, clinicians could begin more aggressive treatments earlier. The new study is published in the journal, Clinical and Translational Medicine.
This is one of the most long-term and comprehensive molecular studies of prostate cancer progression. The slow progression of the disease makes studying its biology difficult.
The bank of biopsies maintained for the last 20 years at Garvan and St Vincent’s Hospital, allowed the researchers to analyze samples from 185 men who had their prostate removed due to a prostate cancer diagnosis in the 1990s and 2000s. The team then tracked the number of men who survived, and those who died from the disease, some more than 15 years later.
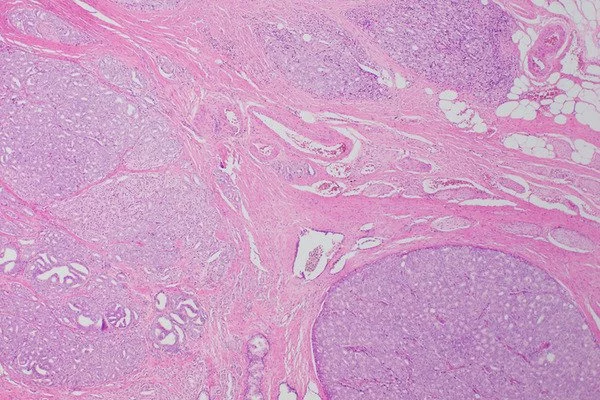
The researchers looked at their genomes and identified 1420 regions specific to prostate cancer where they could see epigenetic changes – marks on the DNA, known as DNA methylation. The methylation process can turn a gene’s activity up or down without altering its DNA sequence like a mutation does.
Of those regions, 18 genes were studied further, with one, the CACNA2D4 gene, which is involved in calcium channel regulation, standing out as a key biomarker.
“We know very little about this gene and it’s not typically profiled, so we really need to understand how the methylation process may suppress the gene’s activity,” says Dr. Ruth Pidsley, the study’s first author.
The comprehensive epigenome sequencing data has been made available to other researchers for use in future prostate cancer research by the team. Not only did the epigenome analysis reveal differences between men with lethal and non-lethal prostate cancer, but the biomarkers also improved existing clinical tools for prognosis.
The new findings offer hope for a more personalized cancer treatment.
“What you really want to know on the day a patient is diagnosed is who has the potential for lethal prostate cancer and who doesn’t, because it will change the way you treat the cancer,” says Professor Lisa Horvath, the clinical lead on the study and an oncologist and researcher at Garvan. “These epigenetic biomarkers have the potential to help us figure out who has lethal prostate cancer and who doesn’t right away,” she says. The next step is to expand the study and see if the biomarkers can be detected in blood samples at the outset.