Researchers at the National Institutes of Health have discovered a new blood test that can be used to quickly assess the severity of pulmonary arterial hypertension (PAH) patients’ condition and forecast survival. A rare, potentially fatal illness called PAH results in unexplainedly high blood pressure in the lungs.
The test greatly outperformed more traditional diagnostics, some of which utilize intrusive instruments, according to early clinical investigations conducted by the researchers. The brand-new blood test quantifies DNA fragments released by harmed cells.
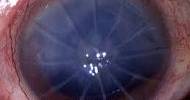
A specific form of pulmonary hypertension called pulmonary arterial hypertension (PAH) is brought on when the small arteries in your lungs thicken and narrow. This constriction restricts blood flow through the lungs, increasing pulmonary blood pressure. Because of this, our hearts have to work harder, and as a result, they become less and less capable of adequately pumping blood throughout the body.
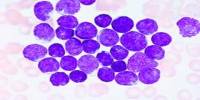
These fragments, known as cell-free DNA, were discovered to be higher in the blood of PAH patients and to rise with the severity of the condition. If additional research supports the results, this ground-breaking blood test for PAH patients may enable medical professionals to act more quickly to stop or slow the disease’s progression and perhaps even save lives.
The prospective medical applications of cell-free DNA, a relatively new analytical technique, are expanding. These applications include the early diagnosis of cancer as well as the rejection of heart and lung transplants.
There is no known precise cause of PAH. It differs from other types of pulmonary hypertension when underlying heart or lung illness is the source of elevated blood pressure in the lungs. According to research, lung blood vessel disease known as PAH is caused by damage to the cells that lining the blood vessels of the lung.
The study was funded by the National Heart, Lung, and Blood Institute (NHLBI) and the NIH Clinical Center, both part of NIH. The findings will appear online in the journal Circulation, a publication of the American Heart Association.
Researchers have been actively searching for novel, less-invasive approaches to evaluate PAH severity, disease progression, and response to therapy for more than a decade. These cell-free DNA analyses represent progress toward that goal.
Michael A. Solomon
A rare kind of pulmonary hypertension called PAH can impair breathing and result in weariness and chest pain. The NIH’s Genetic and Rare Diseases Information Center estimates that less than 50,000 persons in the United States have the condition, whose precise cause is unknown.
Small pulmonary arteries in the lungs gradually narrow and get blocked, the right side of the heart experiences strain, and the patient eventually passes away from heart failure. When lung damage is severe, lung transplantation may be necessary.
The majority of PAH patients are female, and the illness has a significant mortality rate. Despite improvements in treatment, there is currently no cure. The current methods for assessing the severity of PAH rely on known risk prediction scores based on clinical symptoms and on the intrusive use of a catheter to detect lung pressure.
The pressures in the heart are occasionally used by doctors as a proxy for the pressures in the lungs, but these tests typically lack sensitivity and repeatability.
“Researchers have been actively searching for novel, less-invasive approaches to evaluate PAH severity, disease progression, and response to therapy for more than a decade. These cell-free DNA analyses represent progress toward that goal,” said study co-author Michael A. Solomon, M.D., M.B.A., who is part of the NHLBI Cardiovascular Branch and co-director of the NIH Clinical Center Pulmonary Arterial Hypertension Section.
Sean Agbor-Enoh, M.D., Ph.D., study co-author and chief of the NHLBI’s Laboratory of Applied Precision Omics, agreed. “Here we’re proposing a one-time test where you collect a vial of blood from a patient and use that to predict survival. We’re very encouraged by the early results.”
The research team examined cell-free DNA from blood samples collected from 209 adult patients, mostly women, who had been diagnosed with PAH at two major U.S. medical facilities.
The results were contrasted with cell-free DNA obtained from 48 healthy volunteers without PAH who served as a control group and was assessed at the NIH Clinical Center. They discovered that the amounts of cell-free DNA were raised in patients with PAH and rose proportionately to the disease’s severity.
According to the researchers, patients with the highest levels of cell-free DNA had a 3.8 times higher risk of dying or needing a lung transplant than patients with the lowest levels.
Additional examinations of cell-free DNA samples revealed that PAH had an impact on a variety of tissue types, including the heart, blood vessels, adipose tissue, and inflammatory cells flowing through the circulation.
Researchers will be able to more precisely identify the precise tissues involved in the PAH disease process thanks to the new blood test. This information could result in the development of new drugs to treat PAH, whose present therapies only slow the disease’s course rather than halting it or reversing it.
In addition to funding from the Intramural Research Program of the NHLBI, this research is supported by the NIH Clinical Center Research Award for Staff Clinicians Program, the NIH Distinguished Scholar Award, the Lasker Clinical Research Scholars Program, and the Intramural Research Programs of the NIH Clinical Center.