A mouse study that looked at the variations between two variants of the protein PPARgamma, which is a target of ‘glitazone’ diabetes medicines, found that they could reduce weight gain adverse effects.
Researchers from the University of Pennsylvania’s Perelman School of Medicine may have discovered a way to reduce the danger of weight gain associated with a certain type of diabetic medicine by identifying a tiny difference between two versions of a protein. This could lead to more individuals with diabetes receiving more effective therapy from modified thiazolidinediones, which are now avoided due to side effects. These findings were reported in the journal Genes and Development.
“One minor, previously unknown change between two variants of a single protein proved to be quite significant,” research senior author Mitchell Lazar, MD, Ph.D., the Willard and Rhoda Ware Professor of Diabetes and Metabolic Diseases at Penn, said. “Our findings point to a strategy to modify the mechanism of action of thiazolidinedione medicines, which has the potential to eliminate the adverse effect of weight gain.”
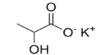
The popularity of diabetes drugs called thiazolidinediones, which are also known as glitazones, has been reduced because of side effects such as weight gain. They work by activating a fat cell protein called PPARgamma (PPARγ). The protein occurs in two forms, PPARγ1 and PPARγ2, whose functional differences have been unclear. But when the Penn researchers examined each form of the protein on its own, they found that activating just PPARγ2 with a thiazolidinedione drug protects mice from diabetes-like metabolic changes — without causing weight gain.
Our findings point to a strategy to modify the mechanism of action of thiazolidinedione medicines, which has the potential to eliminate the adverse effect of weight gain. The finding, therefore, suggests that it may be possible to realize the benefits of thiazolidinediones without the weight gain side effect, by activating only PPARγ2 and not PPARγ1.
Mitchell Lazar
Type 2 diabetes is characterized by the gradual malfunction of the body’s insulin hormone signaling system, resulting in chronically high levels of glucose (sugar) in the blood. This, in turn, contributes to artery hardening, high blood pressure, heart attacks, strokes, and other dangerous disorders. Type 2 diabetes has grown epidemic in many countries and is thought to be caused primarily by obesity, bad diets, and modern sedentary lifestyles. According to the Centers for Disease Control and Prevention, over 35 million people, or roughly 10% of the population, are living with the disorder in the United States alone.
Thiazolidinediones, which include rosiglitazone (marketed as Avandia), were developed in the 1990s and were widely used as diabetes medications for many years. They have since become less popular as a result of its adverse effects. As a result, some researchers are investigating if new molecules may be produced that retain the therapeutic properties of current medications while having fewer negative effects.

Diabetes causes long-term damage to major and tiny blood arteries, which can lead to heart attacks and strokes, as well as problems with the kidneys, eyes, feet, and nerves. The good news is that the danger of diabetes’s long-term complications can be decreased. Regular screening is critical for detecting diabetes-related health issues early. It’s also critical to keep your waist circumference, blood pressure, blood glucose levels, HbA1c, and cholesterol within the prescribed ranges. If you have diabetes, it is critical that you do not smoke because it raises the probability of health problems.
In their study, Lazar and his team approached this problem by taking a closer look at thiazolidinediones’ target, PPARγ, which helps control fat cell production. The scientists studied two lines of mice: One is greatly deficient in one form of the protein, PPARγ1, the other is greatly deficient in PPARγ2. In the mice, the scientists showed that activating PPARγ1 or PPARγ2 with a thiazolidinedione had an anti-diabetic effect in each case, protecting mice from the metabolic harm of a high-fat diet.
However, the researchers discovered that activation of these two forms has subtly different downstream effects on gene activity. Specifically, in the PPARγ1-deficient mice (in which most of the present PPARγ takes the form of PPARγ2), the thiazolidinedione treatment caused no weight gain.
The finding, therefore, suggests that it may be possible to realize the benefits of thiazolidinediones without the weight gain side effect, by activating only PPARγ2 and not PPARγ1. “We’re now studying in more detail how PPARγ1 and PPARγ2 work and how they differ, in the hope of finding ways to selectively activate PPARγ2,” Lazar said.
The American Diabetes Association, the American Heart Association, the Cox Medical Institute, the JPB Foundation, and the National Institutes of Health all contributed to the study.