Mycobacteria are harmful bacteria that cause diseases in humans such as leprosy and tuberculosis. Mycobacteria are connected with red blood cells at lung infection sites, according to a recent study by Hiroshima University scientists, a connection that has escaped scientific awareness for 140 years since the discovery of the organism that causes tuberculosis.
The new study, which was published in Microbiology Spectrum on March 16, 2022, offered light on the interaction of mycobacteria with red blood cells and its function in lung disease.
Discovery of mycobacteria
Robert Koch, a German doctor, discovered the germ that causes tuberculosis (TB) in 1882 and named it Mycobacterium tuberculosis. His findings backed up earlier evidence from French doctor Jean-Antoine Villemin that tuberculosis could be transmitted.
While it would take another 65 years for streptomycin to be used to treat tuberculosis, Koch’s discovery of the bacterial cause prepared the ground for its treatment.
Macrophages, white blood cells that engulf and kill infections, are now recognized to harbor Mycobacterium TB and other mycobacteria implicated in lung illness. Mycobacteria can be found in the blood and sputum of sick people.
Says lead study author and associate professor Yukiko Nishiuchi, “Pathogenic mycobacteria, such as Mycobacterium tuberculosis, Mycobacterium avium subsp. hominissuis (MAH), and Mycobacterium intracellulare, cause pulmonary infections as intracellular parasites of macrophages.”
Our research will change the conventional common sense that mycobacteria grow intracellularly. Their goal is to contribute to development new therapies by better understanding how pathogenic mycobacteria navigate host defense systems to spread.
Yukiko Nishiuchi
The mycobacteria grow inside macrophages. Although red blood cells have been identified in tuberculosis patients’ sputum, they have not been examined in relation to disease progression.
Investigating the role of red blood cells
Lung tissue samples were acquired from five mice infected with two species of Mycobacteria, M. avium and M. intracellulare, as well as a human patient with an MAH infection.
In both the capillary arteries and granulomas (clumps of immune cells) of mice and human lung tissues, microscopic analysis revealed red blood cells co-existing with mycobacteria.
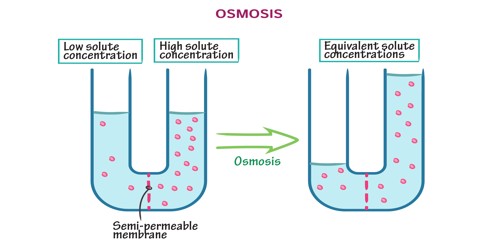
The researchers studied the mycobacteria’s growth in the presence and absence of human red blood cells in order to determine their connection with the cells. They discovered that MAH multiplied at a pace that was dependent on the concentration of red blood cells when it was present. Their exponential growth was even faster than MAH’s within macrophages.
“These results demonstrate that the erythrocytes promoted the vigorous growth of MAH,” says Nishiuchi.
Furthermore, macrophages, which are generally used by mycobacteria as parasitic hosts, were discovered to preferentially devour red blood cells with MAH attached. The MAH binding to red blood cells may have resulted in the release of energy in the form of ATP, causing macrophages to engulf the infected cells.
Implications for human health
The research revealed that pathogenic mycobacteria adhere to human red blood cells and subsequently grow by exploiting the interaction. Mycobacteria had previously been seen outside macrophages at infection sites; however, the latest findings show that the existence of extracellular mycobacteria may be due to the connection with red blood cells.
While red blood cells are best recognized for delivering oxygen from the lungs to the tissues, they also have two functions in mycobacterial infections. They fight infections by catching pathogens and transporting them to macrophages in the liver and spleen, where they are eliminated. This research suggests that mycobacteria may target red blood cells as a host cell.
The way these roles are played could have an impact on the infection’s prognosis. TB or other mycobacterial disease is controlled if the red blood cells’ defense job is effective. However, red blood cells that have been overrun by mycobacteria may aid them spread throughout the body.
Next Steps
The researchers seek to find the adhesion factor that causes mycobacteria to adhere to red blood cells. The adhering mechanism could reveal how mycobacteria, which are normally parasitic inside macrophages, can thrive outside of them.
Says Nishiuchi, “Our research will change the conventional common sense that mycobacteria grow intracellularly. Their goal is to contribute to development new therapies by better understanding how pathogenic mycobacteria navigate host defense systems to spread.”