Social isolation and loneliness have been linked to an increased risk of heart failure. Studies have shown that people who experience these factors have a higher likelihood of developing cardiovascular disease and other health problems, potentially due to increased levels of stress, inflammation, and decreased physical activity. It is important for individuals to maintain social connections and engage in activities that promote physical and mental well-being to reduce the risk of heart failure and other health issues.
According to a new study, both social isolation and loneliness are associated with an increased risk of heart failure, but whether or not a person feels lonely is more important in determining risk than whether or not they are actually alone.
Although research has shown that social isolation and loneliness are risk factors for cardiovascular disease, little is known about their specific relationship with heart failure. According to a new study published in JACC: Heart Failure, both social isolation and loneliness are associated with higher rates of heart failure, but whether or not a person feels lonely is more important in determining risk than whether or not they are truly alone.
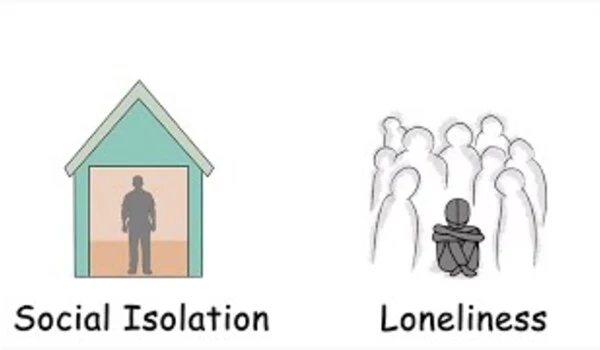
Social disconnection can be classified into two different, but connected components. “Social isolation” refers to being objectively alone or having infrequent social connections, while “loneliness” is defined as a painful feeling caused when someone’s actual level of social interaction is less than they would like it to be.
These findings indicate that the impact of subjective loneliness was more important than that of objective social isolation. These results suggest that when loneliness is present, social isolation is no more important in linking with heart failure.
Jihui Zhang
Researchers examined data from the UK Biobank study, which tracked population health outcomes over a 12-year period and assessed psychosocial factors such as social isolation and loneliness using self-reported questionnaires. The study looked at health outcomes for over 400,000 middle-aged and older adults. Previous studies have been inconclusive, with inconsistent results and different measurements for assessing social isolation and loneliness, according to Jihui Zhang, MD, Ph.D., senior author of the study and a researcher at Guangzhou Medical University in Guangzhou, China.
The researchers discovered that social isolation and loneliness both increased the risk of heart failure hospitalization or death by 15% to 20%. They also discovered that social isolation was only a risk factor when loneliness was not present. In other words, if a person was both socially isolated and lonely, loneliness took precedence. Even if the person was not socially isolated, loneliness increased risk. Men were more likely to be lonely and socially isolated, and they were also associated with negative health behaviors and statuses, such as tobacco use and obesity.
One reason for these findings might be that people can feel lonely even when they are in relationships or interact with others, Zhang said.
“These findings indicate that the impact of subjective loneliness was more important than that of objective social isolation,” he said. “These results suggest that when loneliness is present, social isolation is no more important in linking with heart failure. Loneliness is likely a stronger psychological stressor than social isolation because loneliness is common in individuals who are hostile or have stressful social relationships.”
Zhang said the study pointed to the need for effective tools to screen for social isolation and loneliness in routine clinical care and a broader push to provide more social support. It also indicates the importance of distinguishing between these two factors.
“We will pay more attention to those who are lonely in order to intervene,” he said. “We will screen for social isolation in individuals who do not feel lonely.”
According to him, the findings are especially pertinent because the COVID-19 pandemic has highlighted the effects of social isolation and loneliness on a wide range of health outcomes. Sarah J. Goodlin, MD, a researcher at Patient-Centered Education and Research, and Sheldon Gottlieb, MD, associate professor of medicine at Johns Hopkins University School of Medicine, wrote in a related editorial comment that social isolation and loneliness are frequently influenced by an individual’s socioeconomic status.
“The relationship with social isolation and loneliness is probably strongest in people who are at the extremes of social isolation and loneliness, compounded by low socioeconomic status,” Goodlin and Gottlieb wrote. “Because social determinants of health are increasingly recognized as important components of patient-centered health care, specific interventions, such as ‘social prescribing,’ may be appropriate to incorporate into care.”
Future research will look into the effects of social isolation and loneliness on major health outcomes in vulnerable populations, such as Type 2 diabetes patients, as well as experimental studies to better understand the mechanisms by which social isolation and loneliness affect cardiovascular health.