Obesity and obesity-related metabolic syndromes are global health issues. A growing body of evidence suggests that chronic inflammation is a key feature of obesity and that chronic inflammation can lead to obesity and obesity-related metabolic diseases.
A new pharmacological approach to reducing the mitochondrial dysfunction that promotes diet-induced obesity in mice has been discovered by researchers. A team of scientists from the University of California, Irvine, has developed a novel pharmacological approach to reducing the mitochondrial dysfunction that causes diet-induced obesity. The findings of their study were recently published in the journal EMBO Molecular Medicine.
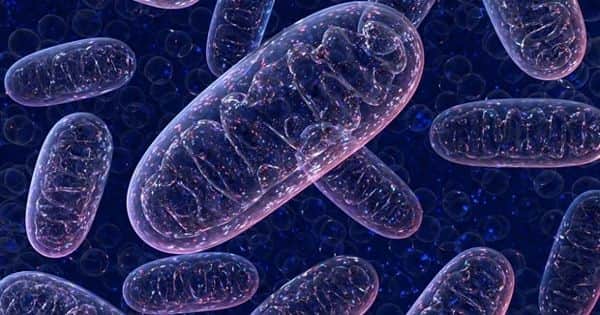
Obesity and metabolic disorders such as diabetes and fatty liver can result from a high-fat diet. Palmitate, a fat commonly found in the Western diet, causes metabolic dysfunction by causing excessive mitochondrial fission within cells. Mitochondria not only play an important role in energy production in cells, but they also coordinate cell stress responses. In some tissue types, excessive mitochondrial fission impairs their function, undermining metabolism and increasing toxic byproducts associated with insulin resistance.
Scientists have discovered a novel pharmacological approach to attenuate the mitochondrial dysfunction that drives diet-induced obesity.
“Elegant genetic studies in mice show that keeping mitochondrial networks fused can prevent obesity caused by a high-fat diet. Our research employs a small molecule to reshape mitochondria in multiple tissues at the same time, reversing obesity and correcting metabolic disease in mice while they continue to consume an unhealthy diet “Aimee Edinger, Chancellor’s Fellow and professor of developmental and cell biology at UCI, is the senior author.
Professor Edinger and her colleagues used their patented water-soluble, orally bioavailable synthetic sphingolipid SH-BC-893 to inhibit endolysosomal trafficking proteins required for mitochondrial fission in their new study.
In vitro experiments and a high-fat diet-induced obesity mouse model were used in the study. SH-BC-893 was found to prevent mitochondrial dysfunction in the liver, brain, and white adipose tissue of mice fed a Western diet. As a result, circulating levels of key metabolic hormones, leptin, and adiponectin, were normalized, resulting in weight loss, improved glucose handling, and reversal of fatty liver disease despite continued access to high-fat food.

Obesity occurs when the amount of energy consumed exceeds the amount of energy expended. While most current obesity treatments focus on caloric restriction, new research suggests that increasing cellular energy expenditure (bioenergetics) may be an appealing alternative approach. This is especially true for adaptive thermogenesis, which is the physiological process by which energy is dissipated as heat in response to external stimuli. Significant recent advances have been made in identifying factors that control the development and function of these tissues, as well as techniques for measuring brown fat in adult humans.
“Obesity-related hormonal imbalances in leptin and adiponectin make it difficult for people to lose weight. Excess leptin can increase appetite, whereas insufficient adiponectin activity has been linked to a variety of metabolic diseases. It is unclear how or why, but the state of the mitochondria may be an important link between these hormones and obesity “said Elizabeth Selwan, co-lead author of the study and a former graduate student researcher in UCI’s Department of Developmental and Cell Biology.
The findings of the study suggest that SH-BC-893 could be a promising therapy for diet-induced obesity. The drug was found to be safe and effective in the mouse model, and the authors intend to further investigate the compound for possible use in human patients.
“This compound works through a novel mode of action; if it is safe and effective in humans, it would provide a new weight loss strategy that could also be combined with other treatments,” Professor Edinger explained.
Obesity occurs when the amount of energy consumed exceeds the amount of energy expended. A small portion of nutrient energy intake is lost in feces and urine; a portion is used for physiological needs (growth, pregnancy, or lactation); a variable, and unfortunately decreasing, a portion is used in physical activity, and the majority is used for metabolic processes or is lost in heat production.