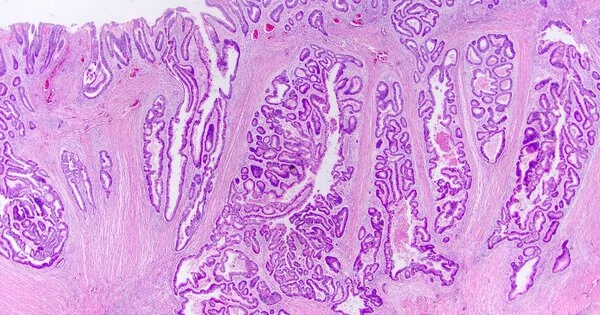
Cancer is a complicated disease, and researchers are continually experimenting with new ways to target and treat various types of cancers, including colon cancer. One cancer therapy strategy is to identify specific proteins or pathways that are important in the growth and survival of cancer cells and then design medicines to target them. These targeted medicines have the potential to interrupt the pathways that fuel tumor development and progression.
Scientists found a previously unknown protein interaction that is crucial for giving energy to tumor cells and could have significant ramifications for the development of future colon cancer treatments.
A team of scientists at VCU Massey Cancer Center discovered a previously unknown interaction between proteins that is responsible for supplying energy to tumor cells in a study published Friday in Cell Reports, which could have significant implications for the development of future treatments for colon cancer.
“This study is really exciting because we may be able to use these findings to inform the development of an entirely new cancer drug right here at Massey,” said study author Can Senkal, Ph.D., a member of Massey’s Cancer Biology research program and an assistant professor in the VCU School of Medicine’s Department of Biochemistry and Molecular Biology.
This study is really exciting because we may be able to use these findings to inform the development of an entirely new cancer drug right here at Massey.
Can Senkal
Ceramides are a type of fatty molecule that may hold the answer. Ceramides govern a variety of critical cellular activities, and many cancer medicines promote ceramide production to aid in disease resistance. Cancer cells can survive and proliferate more efficiently when ceramide formation is reduced.
Senkal and his colleagues began intensively screening cells in the lab to determine which proteins interact with ceramide-producing proteins on a regular basis in order to find potential patterns that justify further examination. Ceramide synthases, the enzymes responsible for ceramide production, are available in six different flavors: Ceramide synthase 1 through 6.
Senkal’s team discovered that the first taste, ceramide synthase 1 (CerS1), was highly interacting with a protein known as heat shock protein 27 (Hsp27). Heat shock proteins operate as chaperones for other proteins, allowing them to function normally; nevertheless, an excess of them might tip the scales and prohibit ceramide synthases from doing their work.
The researchers also discovered that Hsp27 activity was much higher in many colon cancer cells whereas CerS1 activity was significantly lower, causing Senkal and his colleagues to wonder if the absence of one was related to the presence of the other.
“There is this yin-yang kind of relationship, which gave us the idea to follow it,” Senkal said. “Hsp27 is like the bad guy holding back the good guy, CerS1.”
Through the study, they identified a specific biological mechanism through which Hsp27 interacted with and inhibited the function of CerS1 in colon cancer cells. By deliberately blocking the activity of Hsp27 in these cells, the researchers confirmed the decreased presence of Hsp27 led to a heightened reactivation of CerS1, which in turn forced a reduction in mitochondrial function.
“Cancer cells rely on mitochondria for energy in order to multiply. Without it, cancer cells cannot sustain the amount of energy they require and die,” Senkal explained. They were able to reactivate the cellular hand that could pull the plug on the power source attached to the tumour by preventing the action of these heat shock proteins, according to Senkal. This discovery prompted the study’s authors to speculate that Hsp27 could be a main target in the development of innovative colon cancer therapeutics.
“We can really go after these protein-protein interactions and precisely reactivate certain enzymes while we don’t touch others,” Senkal said. These findings are the result of a decade’s worth of research by Senkal and his team, in an area which he noted isn’t really being explored by anyone else.
Senkal recognizes that this will not be an overnight success, but he hopes to engage with other Massey scientists in a long-term effort to adapt these discoveries to in-house innovative medication development at the cancer center. Although this study revealed promising findings in colon cancer, the researchers intend to expand the scope of this research to other solid tumors where Hsp27 overexpression has been detected, such as lung, pancreatic, and prostate malignancies.
“We hope to demonstrate this connection in other tumors as well, which might better represent the patient population in Massey’s catchment area,” Senkal said.
The National Cancer Institute officially named Massey as a Comprehensive Cancer Center, the highest level of designation available that recognizes a center’s scientific leadership, depth and breadth of research, successful community engagement, and cancer research training and teaching.