If germinal centers, which are tiny biological structures, are the immune system’s arsenals, producing antibodies to combat harmful pathogens, then B cells are its ammunition factories. These tiny training grounds, which are created in response to infection and vaccination, allow B cells to hone the antibodies they use to defend against particular viruses and bacteria.
Understanding immunity and creating more potent vaccines consequently require an understanding of how germinal centers function. A recent study published in Cell explains why some germinal centers survive for months as opposed to just a few weeks, offering knowledge that may help with the development of future vaccines.
Old bottle, new wine
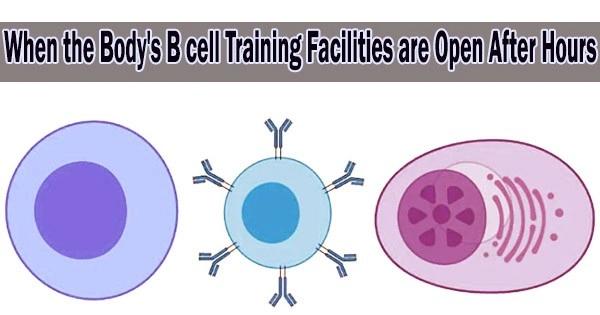
Within a few days of an infection or immunization, germinal centers develop in the lymphatic tissues of the body. B cells rapidly mutate once inside a germinal center, and only B cells with antibodies that most tightly bind to their target antigens survive as a result of natural selection. These more advanced B cells then differentiate into either memory B cells, which scour the body for clues that the disease they were designed to combat is making a comeback, or plasma cells, which are antibody factories that produce massive numbers of antibodies into serum.
“The goal of the germinal center is to generate high-affinity plasma cells and memory B cells, that it then exports,” says Renan V.H. de Carvalho, a postdoctoral fellow in the laboratory of Gabriel D. Victora at The Rockefeller University.
Most germinal centers in mice shut down a few weeks later after successfully creating high-affinity B lymphocytes. However, those that develop as a result of some respiratory diseases, such as the flu, can remain active for more than six months, or about a fifth of a mouse’s typical lifespan. De Carvalho and his associates were interested in learning why these germinal centers persist for such a long time and what what occurs inside of them.
The invasion of ongoing germinal center structures by sequential waves of B cells may turn out to be an important factor in predicting germinal center outcomes, possibly well beyond this particular influenza model, and might give us some insight into how to coax germinal centers to produce the antibodies we need them to.
Gabriel D. Victora
In order to conduct the study, the scientists first infected mice with the influenza and SARS-CoV-2 viruses, allowed them to develop germinal centers, and then sequenced the antibody genes of B cells collected from those centers during a 24-week period.
Much to their astonishment, they discovered that antibody optimization peaked after 12 weeks and then appeared to regress, even if the center was still active, as opposed to continuing evolving at a steady clip. Researchers ultimately discovered that this perplexing decline was caused by the ongoing entry of undeveloped “naïve” B cells into the germinal centers.
As the weeks and months passed, a clearer picture emerged: the founder B cells that had initially seeded the long-lived germinal centers were gradually being replaced by naive ones, leaving just a small percentage of late germinal centers composed of the B cells’ offspring.
Old-school vs. new-school
The initial B cells in the germinal center did not behave like these new recruits. In spite of the fact that the naive B cells also underwent evolution within the germinal centers, further research revealed that they were unable to create antibodies that could bind to flu or SARS-CoV2 antigens.
“We used to think of infection-induced germinal centers as a single reaction targeting antigens from a particular pathogen,” de Carvalho says. “Apparently it’s not, at least in the case of these long-lived germinal centers.”
However, the few original B cells that were still present at the scene were sufficient to provide effective immunity against the original virus. The researchers showed that many of the memory B cells that started pumping out antibodies were descended from the few founder cells that persisted in germinal centers for many months, and not their naive replacements, when they re-exposed the mice to flu antigens 3 months after they were first infected, effectively simulating a repeat infection or booster shot.
“Even though they constitute a small fraction of the total number of cells later on, the founder cells that stay in the germinal center for a long time are still doing their job,” de Carvalho says.
But just how well those founder B cells do their jobs, and whether naïve recruits cramp their style and reduce their efficacy, remains to be seen. Future studies from the Victora lab will address this question.
The discoveries have already had an impact on how we generally understand how germinal centers function. Understanding the dynamic between founder and naïve B cells could help researchers leverage long-lived germinal centers to produce more effective antibodies against dangerous respiratory viruses, like the flu and SARS-CoV-2.
“The invasion of ongoing germinal center structures by sequential waves of B cells may turn out to be an important factor in predicting germinal center outcomes, possibly well beyond this particular influenza model,” Victora says, “and might give us some insight into how to coax germinal centers to produce the antibodies we need them to.”