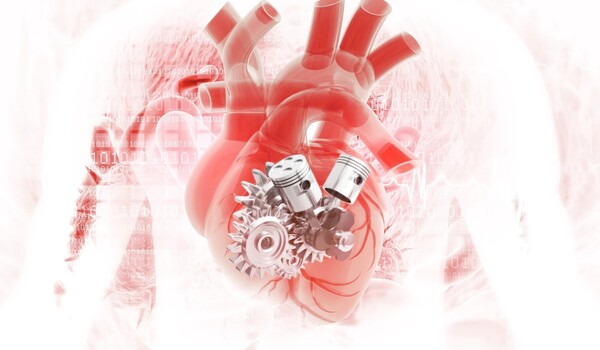
Children born with anomalies affecting the lower chambers of the heart are subjected to a series of invasive procedures at a young age. The first surgery involves the insertion of a shunt, a plastic tube that improves blood flow. However, as children develop, the shunt is frequently updated to fit their growing bodies. Now, researchers have developed a shunt that expands when activated by light. If developed properly, this device could lessen the amount of open-chest procedures these youngsters require.
The researchers plan to report their findings at the American Chemical Society’s (ACS) fall meeting.
“After the surgeon first puts in the tube, these children often have to go through an additional two or three, maybe even four, surgeries just to implant a slightly larger tube,” says Christopher Rodell, who is presenting the research. “Our goal is to expand the inside of the tube with a light-emitting catheter that we insert inside the shunt, completely eliminating the need for additional surgeries.” Rodell is an assistant professor of biomedical engineering at Drexel University.
After the surgeon first puts in the tube, these children often have to go through an additional two or three, maybe even four, surgeries just to implant a slightly larger tube. Our goal is to expand the inside of the tube with a light-emitting catheter that we insert inside the shunt, completely eliminating the need for additional surgeries.
Christopher Rodell
These congenital heart disorders affect the organ’s lower chambers, known as ventricles, limiting blood flow to the lungs and other regions of the body. Without surgery, newborns with severe abnormalities will not survive. These infants, who are frequently born underweight, can grow quickly following their first shunt insertion procedure. To accommodate their growth, doctors frequently undertake another open-chest procedure. This operation puts the youngster at risk every time it is performed. In a study of 360 patients who had their initial heart reconstruction treatment, 41 required subsequent surgeries to implant a bigger shunt, and seven died as a result.
Previously, Rodell’s colleagues at Drexel, Amy Throckmorton and Kara Spiller, built an expandable prototype to potentially replace the most commonly used type of shunt. They did so by coating the interior of the tube with a hydrogel that contains a network of water-surrounded polymers attached to each other by bonds called crosslinks. The formation of new crosslinks forces water out of the hydrogel and pulls the polymers together, contracting the hydrogel and widening the inside of the shunt. In the initial design, the new crosslinks formed automatically, without an external trigger.
Rodell joined Throckmorton and Spiller to help them reengineer the shunt so the materials would be safe for clinical use and so it could be adjusted to meet the needs of individual children. He accomplished this by developing new polymers for a hydrogel that would form new crosslinks and increase the shunt’s inner diameter in response to a trigger. To initiate crosslinking on demand, Rodell decided to use blue light because this wavelength carries enough energy to initiate the reaction but is safe for living tissue.
“Light has always been one of my favorite triggers, because you can control when and where you apply it,” Rodell says.
For the new device, Rodell and his team led by graduate student Akari Seiner are using a fiber-optic catheter, essentially a long, thin tube with a light-emitting tip. To activate the light-sensitive hydrogel inside the shunt, they intend for surgeons to insert the catheter into an artery near the armpit then maneuver it into position, eliminating the need to open the baby’s chest.
In lab trials, they discovered that they could gradually expand the shunt, with the degree of expansion varying depending to the time of light exposure — implying that once implanted, adjustments to the shunt might be tailored to each child. They discovered that they could dilate the shunt by up to 40%, increasing its diameter from 3.5 millimeters to 5 millimeters, closely matching the size of the greatest shunt placed in infants. They also investigated how blood cells and blood arteries might react to the redesigned shunt. They discovered no evidence that the implanted tube caused blood clots, an inflammatory response, or any other potentially harmful effects.
The team intends to test full-length shunt prototypes in an artificial setup that mimics the human circulatory system. If these experiments prove successful, the researchers plan to move on to animal models. Rodell believes that this method could be useful for more than only single-ventricle heart problems. Surgeons could use similar tubes to restore blood arteries in children who have been wounded in a car accident.
“In these procedures, you run into the same problem: Children aren’t just tiny adults; they continue to grow,” Rodell explains. “That’s something we need to account for in biomaterials, how that graft will behave over time.”