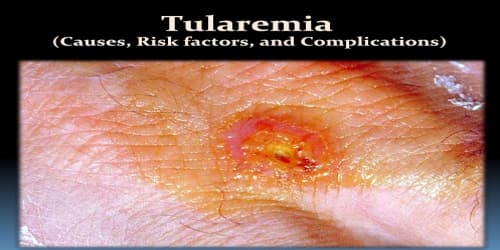
Tularemia (Causes, Risk factors, and Complications)
Definition: Tularemia, also known as rabbit fever, is a rare infectious disease that typically attacks the skin, eyes, lymph nodes and lungs. Symptoms may include fever, skin ulcer, and enlarged lymph nodes. Occasionally, a form that results in pneumonia or a throat infection may occur.
Tularemia is an infectious disease that typically infects:
- wild rodents
- squirrels
- birds
- rabbits
Humans can become infected through several routes, including:
- Tick and deer fly bites
- Skin contact with infected animals
- Ingestion of contaminated water
- Inhalation of contaminated aerosols or agricultural dust
- Laboratory exposure
In addition, humans could be exposed as a result of bioterrorism.
The various forms of tularemia are distinguished by where the bacteria enter the body. The most common form of the disease is caused by skin contact with the bacteria. The deadliest form of the disease is caused by inhaling the bacteria.
Tularemia can often be treated with antibiotics. Early treatment offers a good outlook for complete recovery. However, some severe cases may be fatal even with treatment.
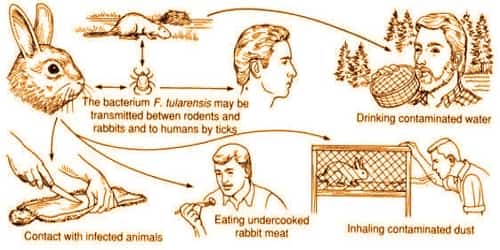
Causes and Risk factors of Tularemia: Tularemia is caused by the bacteria Francisella tularensis which is typically spread by ticks, deer flies, contact with infected animals. However, tularemia occurs worldwide, especially in rural areas. The organism can live for weeks in soil, water, and dead animals.
In general, People can get tularemia through:
- Insect Bites
- Exposure to sick or dead animals
- Airborne bacteria
- Contaminated food or water
Skin exposure is the most common form of the disease. Inhalation through the lungs is the deadliest form of tularemia. If it’s left untreated, other forms of the disease may eventually reach the:
- lungs
- spinal cord
- brain
- heart
The disease can cause serious complications and sometimes death.
Although anyone of any age can develop tularemia, engaging in certain occupations or activities or living in certain areas pose a greater risk.
People at an increased risk for tularemia include:
- those who work closely with animals, such as veterinarians, zookeepers, and park rangers
- those who live in heavily forested areas
- those who work with animal carcasses, such as hunters, taxidermists, and butchers
- those who work in gardening and landscaping
Cats and dogs can acquire the disease from the bite of a tick or flea that has fed on an infected host, such as a rabbit or rodent. For treatment of infected cats, antibiotics are the preferred treatment, including tetracycline, chloramphenicol or streptomycin. Long treatment courses may be necessary as relapses are common.

Complications of Tularemia: Males are affected more often than females. Tularemia occurs most frequently in the young and the middle-aged. Left untreated, tularemia can be fatal. Other possible complications include:
- Inflammation of the lungs (pneumonia). Pneumonia can lead to respiratory failure — a condition in which the lungs don’t take in enough oxygen, don’t release enough carbon dioxide or both.
- Infection around the brain and spinal cord (meningitis). Meningitis is a serious and sometimes life-threatening infection of the fluid and membranes (meninges) surrounding the brain and spinal cord.
- Irritation around the heart (pericarditis). This is swelling and irritation of the pericardium, the thin membrane that surrounds the heart. Mild pericarditis may improve without treatment, but more-serious cases may require antibiotic therapy.
- Bone infection (osteomyelitis). Tularemia bacteria sometimes spread to the bones.
The tularemia bacterium was first isolated by G.W. McCoy of the United States Public Health Service plague lab and reported in 1912. Scientists determined tularemia could be dangerous to humans; a human being may catch the infection after contacting an infected animal. The ailment soon became associated with hunters, cooks and agricultural workers.
Information Source: