Scientists have discovered a novel therapeutic medication that can overcome antibiotic resistance in bacteria that cause sepsis, pneumonia, and urinary tract infections, among other illnesses.
Carbapenems, such as meropenem, are a class of antibiotics that are often used as a “last option” when other antibiotics, such as penicillin, have failed to treat serious, multi-drug resistant infections. However, certain bacteria have discovered a way to resist carbapenem treatment by creating enzymes known as metallo-beta-lactamases (MBLs), which break down carbapenem antibiotics and prevent them from working.
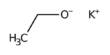
Highly collaborative research, conducted by scientists from the Ineos Oxford Institute (IOI) for Antimicrobial Research at the University of Oxford and several institutions across Europe, found that the new class of enzyme blockers, called indole carboxylates, can stop MBL resistance enzymes working leaving the antibiotic-free to attack and kill bacteria such as E. coli in the lab and in infections in mice.
The European Lead Factory (ELF) and the European Gram-Negative Antibacterial Engine (ENABLE) programs of the Innovative Medicines Initiative (IMI) financed the new study, which was published in Nature Chemistry today (Monday).
The researchers first evaluated hundreds of thousands of compounds to determine which ones would bind strongly to MBLs and not react with any human proteins, which led to the discovery of indole carboxylates as intriguing new options.
The researchers discovered that these potential medications bind to MBLs in a completely different way than any other drug, imitating the antibiotic’s interaction with the MBLs, using a technique called crystallography to zoom in and take a closer look at how they work.
These possible medications are particularly powerful against a wide range of MBL-producing superbugs thanks to this smart Trojan Horse approach.
An increase in antimicrobial resistance is absolutely inevitable. It a massive problem because collectively we haven’t been making enough new clinically useful antibiotics. As a society we must find ways both to make new antibiotics and protect the ones we have. The alternative is that routine modern medicine will be disrupted in a manner simply too horrendous to conceive.
Christopher Schofield
After discovering the medications, the researchers chemically altered them to make them more effective and then tested them in combination with carbapenems against multidrug-resistant bacteria in both lab dishes and animals.
The possible new medications were found to be 5 times more effective at treating severe bacterial infections when used in combination with carbapenems than carbapenems alone, and at a lower dose. Importantly, in mice, these potential medications have only minor adverse effects.
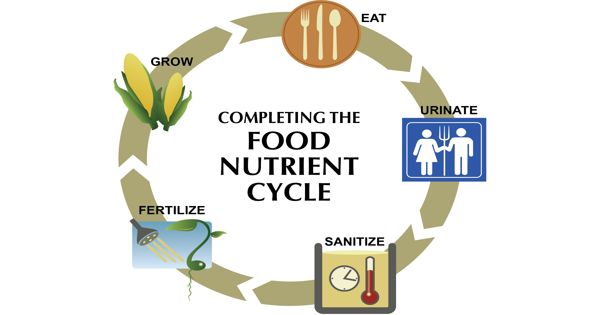
Carbapenems work in the same way that penicillin and other beta-lactam antibiotics do. When bacteria try to grow and proliferate, they are prevented from creating new cell walls, which kills the germs. Carbapenems are more stable than similar antibiotics, and many of the strategies bacteria use to resist antibiotics do not work with carbapenems.
Resistance to carbapenems, on the other hand, evolved from genes that code for MBLs, which can quickly spread from bacteria to bacterium. There is currently no licensed drug that targets MBLs, and only one is in clinical studies, therefore new therapies to overcome resistance, protect carbapenems, and keep these valuable medicines working for longer are urgently needed.
Antimicrobial resistance, according to the World Health Organization (WHO), will cause 10 million deaths per year by 2050, surpassing cancer-related mortality and becoming one of humanity’s most significant health issues.
Professor Christopher Schofield, Academic Lead (Chemistry), Ineos Oxford Institute at the University of Oxford, said:
“An increase in antimicrobial resistance is absolutely inevitable. It a massive problem because collectively we haven’t been making enough new clinically useful antibiotics. As a society we must find ways both to make new antibiotics and protect the ones we have. The alternative is that routine modern medicine will be disrupted in a manner simply too horrendous to conceive.”
“The collaborative efforts of academics and industry scientists have discovered a brand new class of drug that can shut down one of the ways bacteria fight back against antibiotics. This research is the culmination of years of work, from screening huge libraries of chemicals, through to testing the best drug candidates in pre-clinical studies in the lab. We are actively progressing this new drug type towards clinical trials in people, most importantly in lower and middle income countries where resistance to carbapenem antibiotics is widespread.”
Professor Tim Walsh, Academic Lead (Biology), Ineos Oxford Institute at the University of Oxford, said: “Academia, given the space to create, can produce something amazing and that’s what we have seen here. With the fantastic support we have received from INEOS, we can replicate this type of drug discovery programme within the IOI for multiple different bacterial targets and applications.”
“As well as drugs that overcome resistance to current antibiotics, in the IOI we wish to discover entirely new types of antibiotics not only to fight bacteria that cause infections in humans, but in bacteria that affect farm animals. These animals, such as chickens and pigs, are a source of human antimicrobial resistance, so we’re looking to develop drugs to use exclusively in agriculture and help protect against multidrug resistant infections.”