According to experts, the microbiota in the nose and upper neck likely includes indicators for determining how unwell a person infected with SARS-CoV-2 would become and creating novel therapeutic techniques to enhance their prognosis.
According to Dr. Sadanand Fulzele, a geriatric researcher at Augusta University’s Medical College of Georgia, the nasopharyngeal microbiota serves as the first line of defense against viruses, bacteria, and other pathogens that enter these natural pathways.
When the researchers looked at the microbiota of 27 people aged 49 to 78 who were negative for the virus, 30 who were positive but had no symptoms, and 27 who were positive but had moderate symptoms that did not require hospitalization, they discovered distinct patterns, according to a study published in the journal Diagnostics.
“Millions of people get infected and relatively few of them become symptomatic. This might be one of the reasons,” says Dr. Ravindra Kolhe, director of MCG’s Georgia Esoteric and Molecular Laboratory, or GEM Lab. which has performed more than 100,000 COVID tests.
According to corresponding author Fulzele, the most dramatic alterations were in those who were symptomatic, with nearly half of those patients not having enough microbiota to even sequence.
They were startled to discover these “low reads” of bacteria in the nasopharyngeal cavity of symptomatic people, compared to only two and four in the negative and positive with no symptoms groups, respectively. According to lead author Kolhe, “the great majority of the positive patients with no symptoms nevertheless had sufficient microbiota.”
“We don’t know which came first, the disease or the wipeout of the microbiota,” Fulzele says. Runny noses and sneezing may have contributed to the decline, an already low bacterial population may have raised the people’s likelihood of acquiring these symptoms, or the virus may have altered the landscape, according to Fulzele, who believes the latter.
Kolhe believes the varied microbiota composition and size is another solid bet, based on his expertise with bacteria in the gastrointestinal system, and they both want a clear response. “We don’t have sufficient data at this moment,” Kolhe says.
They discovered variations in the types of bacteria as well, however the purpose of some of the bacteria they discovered is unknown, according to the researchers.
A major method for transmitting severe acute respiratory syndrome coronavirus 2, or SARS-Cov-2, is when someone coughs, sneezes, or even talks, and droplets called aerosols carrying the virus move through the air and into another person’s nose or mouth, as the virus’s name and nearly two years of experience with it indicate.
Those age 65 and older and/or with underlying health conditions like hypertension and diabetes are considered at increased risk for hospitalization and death from the infection, so they decided to look at the microbiota in the upper part of the respiratory system called the nasopharynx of older individuals.
According to Fulzele, the wet, mucus-producing lining of this area acts as a natural barrier to intruders, and there is also a substantial complement of immune cells there, which respond to respiratory viruses.
Kolhe adds the region is also rich in ACE-2 receptors, which the spiky virus attaches to, and it’s a key landing place for the virus. According to Kolhe and Fulzele, the changed microbiota in symptomatic individuals influenced their immune response to the infection.
The symptomatic people had considerably greater amounts of two bacterial species, including Cutibacterium, which is commonly found on the skin and linked to acne, as well as heart infections and shoulder infections after surgery. A handful of other, less well-studied bacteria, on the other hand, were found in considerably lower numbers.
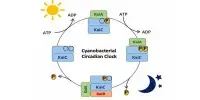
Both symptomatic and asymptomatic infected groups exhibited high levels of Cyanobacteria, commonly known as blue green algae, which can be found in polluted water but is a common resident of the human microbiome and appears to play a role in immune response regulation. These bacteria are known to cause pneumonia and liver damage when they enter the body through mucosal surfaces such as the nose. Those who were sick had double the amount of these bacteria as those who were asymptomatic.
Fulzele observes that there was no substantial difference in microbiota diversity between the asymptomatic and the symptomatic, only large changes in volume, although they did find a lot of specific bacteria going up and down in numbers.
Their graph showing the number of another water-loving bacterium, Amylibacter, for example, appeared like stair steps as it climbed from negative to positive with symptoms people, while a handful of other bacterium showed a downward trend.
While the link between the nasopharyngeal microbiota and COVID-19 severity is unknown, the researchers note that their research shows a “strong association” between the nasal microbiota, SARS-CoV-2 infection, and severity.
Their research was conducted before the current viral variations emerged, but the researchers believe the microbiota differences will hold true for them as well, and they have already begun their investigation.
The researchers suggest that larger investigations are needed to confirm the apparent trends they saw. They’re working on a grant proposal to fund a larger research, and they’re seeking for more testing locations to collaborate with. They claim that by using the same nasopharyngeal swab utilized for several COVID tests, a microbiota study may be performed at the same time as testing.
They point out the dramatic disparity that has arisen after nearly two years of exposure to the virus, with the majority of individuals infected asymptomatic or suffering minor symptoms similar to a cold, while some develop severe viral pneumonia, require hospitalization, and die.
They add that a number of recent research have found that the bacterial makeup of the nasal canal has a “dramatic” impact on the development of respiratory infections and the severity of symptoms. According to certain research, the nasal microbiota can impact the viral load, immune response, and symptoms of a rhinovirus infection, which is responsible for 10-40% of common colds.
They note that a variety of other illnesses, including inflammatory bowel syndrome, peptic ulcers, and viral infections, have been related to substantial alterations in the gut, nasal, and oral microbiota.
According to Fulzele, the diversity of bacteria in the microbiota is usually a positive thing, and it’s something that naturally declines with age. It may also be hurt by behaviors like smoking and helped by habits like eating a varied diet. The National Institutes of Health helped fund some of the research.