T cells, also known as T lymphocytes, are an important component of the immune system that aids in the identification and destruction of cancer cells. In varying cancer types in mouse and human tissue samples, scientists discovered a relationship between the immune system’s killer T cells and the body’s sympathetic stress response (‘fight-or-flight’), discovering that killer T cells and sympathetic stress response hormones interact to ‘exhaust’ killer T cells – but that exhaustion can be inhibited with beta-blockers. The data show that combining beta-blockers with established immunotherapies can improve cancer treatment.
Even for killer T cells, which are specialist immune cells, constantly hunting and eliminating cancer cells can be taxing. Scientists will be able to produce more robust cancer-killing cells if they can grasp why killer T cells become weary.
Salk Institute researchers established a link between killer T cell depletion and the body’s sympathetic stress response (“fight-or-flight”) in several cancer types in mouse and human tissue samples in a recent study. Furthermore, the researchers discovered that the interaction between killer T cells and sympathetic stress response hormones can be inhibited with beta-blockers, a class of drugs already used in humans to control blood pressure and heart rate, in order to generate killer T cells that fight the tumor more effectively.
The innervation of tumors is an understudied area of tumor immunology. Our study has now uncovered that nerves contribute to the process of T cell exhaustion in tumors, where T cells become worn out and less powerful in their fight against the tumor over time.
Anna-Maria Globig
The findings, published in Nature on September 2023, establish a new link between the sympathetic stress response and how the immune system responds to cancer. Additionally, they demonstrate the benefit of pairing beta-blockers with existing immunotherapies to improve cancer treatment by bolstering killer T-cell function.
“There is no doubt that immunotherapy has transformed cancer patient treatment — but it is ineffective for many patients,” says Professor Susan Kaech, senior author and director of Salk’s NOMIS Center for Immunobiology and Microbial Pathogenesis. “Finding that our nervous system can suppress the function of cancer-destroying immune cells opens up entirely new ways to think about how to rejuvenate T cells in tumors.”
The sympathetic nervous system regulates the body’s stress reaction, also known as the fight-or-flight reflex. Little was known, however, about how nerves influence the immune response to infections or malignancies.
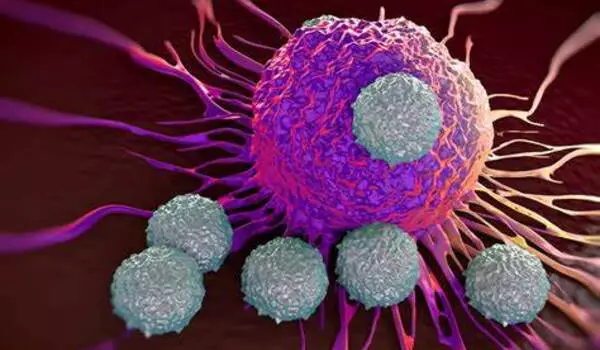
The researchers concentrated on sympathetic nerves, which innervate our organs and create noradrenaline, a messenger hormone that is also a stress hormone. The researchers studied when and how sympathetic nerves regulate killer T cells in mice and human tissue samples using a variety of cancer and chronic illness models.
They discovered that sympathetic nerves produce noradrenaline, which binds to killer T cells via a receptor called ADRB1. Killer T cells that were exhausted expressed more ADRB1 receptors than their functioning counterparts, allowing the T cells to “listen” to the noradrenaline emitted by the nerves.
To see if killer T cell exhaustion could be avoided, the researchers tried two approaches to interfering with noradrenaline and ADRB1 interaction: either completely removing ADRB1 or impairing ADRB1 function with beta-blockers, which resulted in more functional killer T cells that were better at destroying cancer cells.
The researchers also discovered that fatigued T cells do not only listen to neurons from a distance, but congregate immediately around them in tissues. Surprisingly, the ADRB1 receptor gave T cells vital instructions to migrate near the nerves, which reduced their capabilities and made them less effective at combating cancer.
“The innervation of tumors is an understudied area of tumor immunology. Our study has now uncovered that nerves contribute to the process of T cell exhaustion in tumors, where T cells become worn out and less powerful in their fight against the tumor over time,” says first author Anna-Maria Globig, a postdoctoral researcher in Kaech’s lab. “If we can unravel the details of how nerves suppress the body’s immune response to cancer and why the exhausted T cells move towards the nerves, we can begin to target this process therapeutically.”
According to Kaech, the researchers seek to learn more about why stress makes us sick by expanding their understanding of the tired killer T cell milieu. “We were able to find a new pathway that we can target with beta-blockers to create more resilient killer T cells that resist exhaustion and fight cancer better,” Globig explains.
Because beta-blockers are currently in clinical use, the team aims to apply their recommended cancer-fighting regimen in lung cancer patients soon. They intend to analyze more human cancer tissue samples in collaboration with doctors in order to enrich their findings and provide additional proof of the usefulness of beta-blockers in cancer treatment.