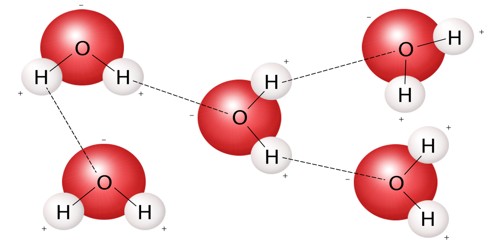
The polymerase chain reaction (PCR), which can identify genetic material such as that from a virus or human DNA, has been the industry standard for molecular diagnostic testing for more than 30 years. A given DNA segment can be quickly multiplied (amplified) into millions or billions of copies using the PCR method, allowing for in-depth analysis.
American biochemist Kary Mullis developed PCR at Cetus Corporation in 1983. Mullis and Michael Smith, who had created other crucial techniques for altering DNA, shared the 1993 Nobel Prize in Chemistry.
However, PCR, particularly reverse transcription polymerase chain reaction (RT-PCR), is often carried out at large, centralized laboratories rather than in point-of-care (POC) settings because the required instrumentation is cumbersome, expensive, and labor-intensive to operate.
Due to these restrictions, there has been a lack of precise POC diagnoses and a backlog in test findings, especially during the COVID-19 epidemic. Many of the techniques used in genetic testing and research, such as the study of ancient DNA samples and the detection of infectious organisms, are fundamentally based on PCR.
Small amounts of RNA from specimens are amplified using PCR technique into deoxyribonucleic acid (DNA), which is duplicated until SARS-CoV-2 is detectable, if present. Since it was permitted to be used in February 2020, the PCR test has served as the gold standard for diagnosing COVID-19.
Researchers from Columbia Engineering and Rover Diagnostics revealed today that they have developed an RT-PCR platform that provides findings faster than existing PCR tests on the market, matching the lengthy laboratory-based testing in 23 minutes.
Our aim was to create a platform that can be used in locations where rapid turnaround results are critical, at pharmacies, transportation hubs, public events, and at companies screening employees coming back to work.
Professor Sam Sia
It can be modified to test for a variety of viruses that call for quick diagnosis, such as COVID-19, the flu, strep, and other viruses in addition to COVID-19. Contrary to isothermal, antigen, and CRISPR testing, its targeted sensitivity is higher.
Additionally, the Rover PCR weighs only two pounds and is user-friendly and portable.
“Our aim was to create a platform that can be used in locations where rapid turnaround results are critical, at pharmacies, transportation hubs, public events, and at companies screening employees coming back to work,” said Sam Sia, professor of biomedical engineering and Vice Provost for the Fourth Purpose and Strategic Impact at Columbia.
The technology was created in collaboration with Rover Diagnostics, a biotech start-up that Sia and Mark Fasciano, the CEO of Rover, co-founded in 2018. The platform avoids the traditional Peltier device approach, which heats the sample from the exterior of the vial, by using sample preparation procedures created in Sia’s lab in conjunction with a new approach to thermal cycling.
Instead, Rover’s solution use a photothermal method called plasmonic thermocycling that depends on light-irradiated nanoparticles to quickly produce heat from within.
In a reaction vessel with all the PCR reagents, the team completed reverse-transcriptase quantitative PCR (RT-qPCR) effectively. The current industry-recognized laboratory method for detecting COVID infection is qPCR. The method allows for infectious unit quantification, but it also presents a number of challenges for point-of-care (POC) downsizing.
In the work that was just published in Nature Nanotechnology, the researchers overcame these difficulties by using plasmonic nanoparticles, which are small metallic particles that emit heat in response to infrared light, enabling real-time and multiplexed RT-qPCR on clinical samples.
“This should really move the needle on delivering rapid and accurate molecular clinical diagnostics in decentralized settings,” said Fasciano, a computer scientist turned software and biotech entrepreneur. “Thermal cycling, so critical to DNA and RNA testing, can now be sped up and clinicians and patients alike won’t have to wait so long for results.”
The COVID-19, its variations, and other infectious disorders are being detected through a commercial device being developed by the Rover team.