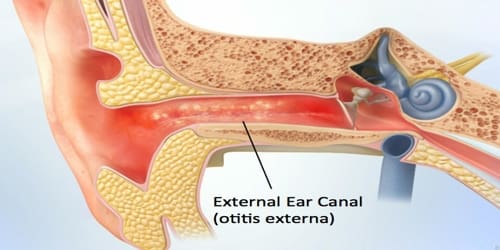
Otitis Externa
Definition: Otitis externa is a condition that causes inflammation (redness and swelling) of the external ear canal, which is the tube between the outer ear and eardrum. It often presents with ear pain, swelling of the ear canal, and occasionally decreased hearing. Typically there is a pain with movement of the outer ear. A high fever is typically not present except in severe cases.
It may develop when water, dirt or other debris gets into the ear canal. Since it is often associated with excess water in the ear canal, and frequently occurs in children and young adults who swim a great deal, the common name for this inflammation is “swimmer’s ear”.
Risk factors for acute cases include swimming, minor trauma from cleaning, using hearing aids and earplugs, and other skin problems, such as psoriasis and dermatitis. People with diabetes are at risk of a severe form of malignant otitis externa. Diagnosis is based on signs and symptoms. Culturing the ear canal may be useful in chronic or severe cases.
Otitis externa is relatively common. It’s estimated that around 1 in 10 people will be affected by it at some point in their lives.
The condition is slightly more common in women than men and is most often diagnosed in adults aged 45 to 75.
Acetic acid ear drops may be used as a preventative measure. Treatment of acute cases is typical with antibiotic drops, such as ofloxacin or acetic acid. Steroid drops may be used in addition to antibiotics. Treatment of chronic cases depends on the cause.
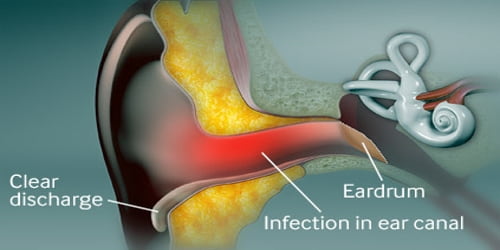
Causes, Sign, and Symptom of Otitis Externa: The two factors that are required for external otitis to develop are (1) the presence of germs that can infect the skin and (2) impairments in the integrity of the skin of the ear canal that allow an infection to occur.
Most cases of otitis externa are caused by a bacterial infection, although the condition can also be caused by:
- Irritation
- Fungal infections
- Allergies
- Seborrhoeic dermatitis
Otitis externa is often referred to as ‘swimmers ear’ because a common cause is a water remaining in the ear canal after swimming. Acute otitis externa is commonly a bacterial infection caused by Streptococcus, Staphylococcus, or Pseudomonas types of bacteria.
Use of products such as bubble baths, shampoos, hairspray and hair dyes can irritate the ear canal and lead to an outer ear infection. Insects may become trapped in the ear. Diabetes is often associated with a particularly severe form of otitis externa.
Otitis externa can cause a number of different symptoms affecting the ear and the surrounding area.
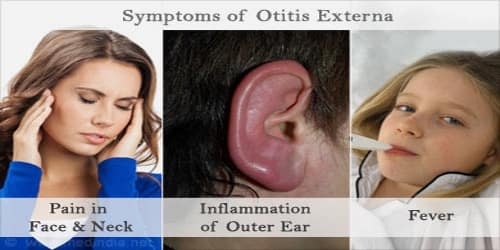
The following are common symptoms of otitis externa:
- Itching and a feeling of fullness inside the ear canal is usually the first sign of infection.
- Swelling of the ear canal
- Watery discharge from the ear
Severe pain and tenderness in the ear – especially when moving the head and jaw, or gently pulling the earlobe. Unlike a middle ear infection (otitis media), the pain of an ear canal inflammation or infection is worse when chewing, when pressing on the “tag” in front of the ear, or when moving the earlobe. The pain also often worsens when the ear starts discharging.
- A foul-smelling, yellowish discharge from the ear
- Temporarily muffled hearing (caused by blockage of the ear canal)
- The ear canal may swell to such an extent that it becomes completely closed.
- Enlarged neck glands which may make it difficult to open the jaw
Otitis externa sometimes occurs if a hair follicle inside the ear becomes infected by bacteria and develops into a spot (a pimple) or boil.
Diagnosis and Treatment of Otitis Externa: The pain worsens or does not improve within 24 hours. In rare cases, the infection can spread and damage underlying bones and cartilage. Patient notice a rash on their scalp or near their ear, they may have seborrheic dermatitis, for which the doctor can provide treatment.
It may be difficult to see the eardrum with an otoscope at the initial examination because of narrowing of the ear canal from inflammation and the presence of drainage and debris. Sometimes the diagnosis of external otitis is presumptive and return visits are required to fully examine the ear.

The diagnosis may be missed in most early cases because the examination of the ear, with the exception of pain with manipulation, is nearly normal. In some early cases, the most striking visual finding is the lack of earwax. As a moderate or severe case of external otitis resolves, weeks may be required before the ear canal again shows a normal amount of it.
Otitis externa can usually be remedied with a simple course of eardrops, as prescribed by patient’s local GP. If their symptoms linger or their case has been particularly severe, they may be referred to a specialist who may undertake, micro-suction or dry swabbing to remove earwax and other debris to make their drops more effective. Severe cases may require an earwick, a plug made from soft cotton gauze that helps insert medication into their ear.
Effective solutions for the ear canal include acidifying and drying agents, used either singly or in combination. When the ear canal skin is inflamed from the acute otitis externa, the use of dilute acetic acid may be painful.
Ear drops are the mainstays of treatment for external otitis. Some prescription drops also contain anti-inflammatory steroids, which help to resolve swelling and itching. Antibiotics by mouth should not be used to treat uncomplicated acute otitis externa. Oral anti-pseudomonal antibiotics can be used in case of severe soft tissue swelling extending into the face and neck and may hasten recovery.
Avoid scratching the inside of the ear or using earbuds, as this will aggravate the irritated skin, and will often make the condition worse. A hearing aid should be left out as much as possible until swelling and discharge stops.
Information Source: