Organ-on-chip (OOC) technology can imitate human organs in vitro, allowing for speedier and more cost-effective medication development while also providing insights into human health. OOC also means that scientists can forgo using animal models in favor of acquiring human-specific, tissue-level, and organ-level data in vitro. OOC research has included kidney, liver, airway, blood-brain-barrier, and heart research, and DARPA has backed the fabrication of an instrument that fluidly connects many OOCs together to create a body-on-chip, allowing researchers to study how medications affect numerous organ systems.
There is currently little research focused on understanding the mechanics of lymphatic vascular disorders and medication discovery. However, disorders such as lymphedema, a buildup of fluid in the body caused by a malfunctioning lymph system, affect more than 200,000 people in the United States alone each year.
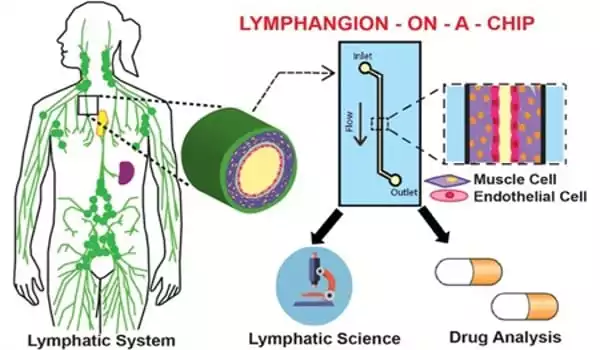
Dr. Abhishek Jain, assistant professor in the Department of Biomedical Engineering at Texas A&M University, has used his experience in organ-on-chip models to a hitherto unexplored field, inventing the first lymphangion-chip.
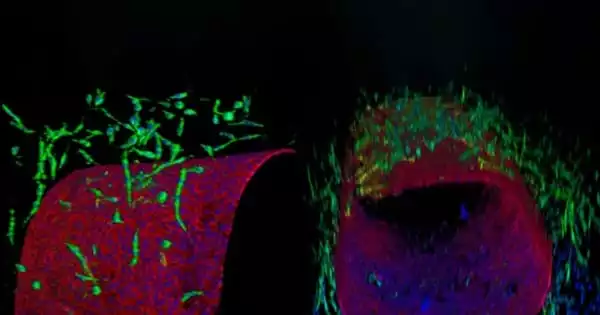
Jain’s team initially devised a new approach for creating microfluidic cylindrical blood or lymphatic tubes made of endothelial cells, which line blood vessels, in order to manufacture this new device. It might then use this technology to successfully duplicate a typical segment of a lymphatic transport conduit in vitro, or outside the body, by creating a co-cultured multicellular lymphangion, the functional unit of a lymph vessel.
The most exciting aspect of this discovery is that it allows us to now push the organ-on-chip in directions where finding solutions for rare and orphan (understudied) diseases is achievable with less work and money. We can assist the pharmaceutical sector in investing in this platform in order to find a solution for lymphedema, which affects millions of people.
Dr. Abhishek Jain
“We now have a better understanding of how mechanical forces control lymphatic physiology and pathology,” added Jain. “We can also understand the mechanisms that cause lymphedema, and then use this platform to find new targets for medication discovery.”
Organs-on-a-chip are gaining popularity as prospective platforms for drug screening and testing. However, alternatives for lymph nodes-on-chip remain limited, despite the fact that the lymph node is one of the primary determinants of the immunotoxicity of newly developed pharmaceutical medicines. We present existing biomimetic lymph nodes-on-chip, their design, and their physiological significance to pharmacology in this review, as well as future directions related with lymph node-on-chip design and implementation in drug discovery and development.
Dr. David Zawieja of Texas A&M College of Medicine is working on the project alongside him. Their findings appeared in the journal Lab on a Chip.
“Collaborations with Dr. Zawieja and other members of the department were critical,” Jain stated. “They introduced me to this topic and provided their longtime experience that allowed us to establish this novel organ-on-chip platform and now push it in these fascinating directions using modern experimental models.”
According to Jain, the importance of this work is far-reaching because it provides new hope for those suffering from lymphatic disorders. They can now learn about the biology of these disorders and progress to the point where they can be treated.
“The most exciting aspect of this discovery is that it allows us to now push the organ-on-chip in directions where finding solutions for rare and orphan (understudied) diseases is achievable with less work and money,” Jain added. “We can assist the pharmaceutical sector in investing in this platform in order to find a solution for lymphedema, which affects millions of people.”
OOC hold significant promise for regenerative medicine, ranging from the replacement of injured tissues and organs to the development of induced pluripotent stem cells. OOC technology has been used to regenerate wounded central nervous system neurons and construct endothelialized human myocardium to help a sick heart, and it may be utilized to create a customized human model, enabling for personalized prevention methods and tailored therapeutics.
Organs-on-a-chip have lately emerged as effective screening techniques in pharmacology and toxicology. When compared to standard tissue culture plates and animal models, such chips allow for more accurate examination of the safety and efficacy of investigational medications. Micromolding, microetching, soft lithography, and photopolymerization are all engineering processes that can be used to create organs on-chip. These approaches have allowed for the creation of incredibly detailed structures that closely mirror those found in the human body, such as the villi of the small intestine and the alveoli of the lungs.