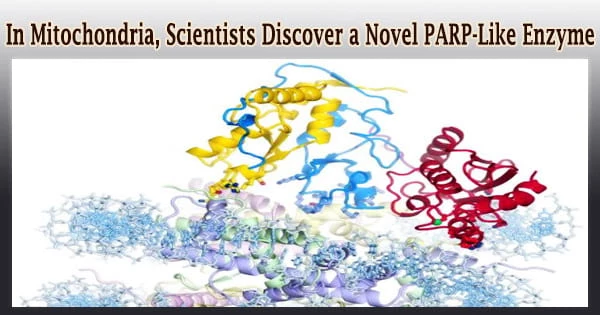
For the first time, Boston University School of Medicine (BUSM) researchers have found and described an ADP-ribosyltransferase enzyme that is active in mitochondria (the organelle that generates the majority of the chemical energy needed to power biological activities in cells).
A biological catalyst, an enzyme is usually always a protein. It accelerates the rate of a particular chemical reaction in the cell. During the reaction, the enzyme is not destroyed and is reused. A cell includes thousands of distinct enzyme molecules, each of which is responsible for a specific chemical reaction.
ADP-ribosyltransferases are enzymes that help other proteins modify themselves. The action of NEURL4, a novel mitochondrial enzyme, is similar to that of PARP1, a nuclear enzyme known for its crucial involvement in DNA damage repair and gene expression regulation.
Mitochondria (plural: mitochondrion) are membrane-bound cell organelles that provide the majority of the chemical energy required to fuel the cell’s metabolic activities. Adenosine triphosphate (ATP) is a tiny molecule that stores the chemical energy created by mitochondria. Mitochondria have tiny chromosomes of their own.
Enzymes are biological catalysts that are usually proteins but can also be RNA. The purpose of a catalyst is to speed up the rate at which a reaction occurs. And the genome encodes a large number of enzymes that produce proteins or RNAs that speed up chemical reactions and perform thousands of distinct functions inside a cell.
While this will not directly improve people’s quality of life, we hope it will provide fertile grounds for new translational applications for the treatment of diseases with a mitochondrial component, such as cancer, diabetes, age-related neurodegenerative disorders, and rare mitochondrial diseases.
Valentina Perissi
The team led by first and co-corresponding author Maria Dafne Cardamone, Ph.D., a former research assistant professor of biochemistry at BUSM, used in-vitro enzymatic tests to evaluate the enzymatic activity of NEURL4.
Then, using a gene-editing method, scientists created a cell line in which NEURL4 was deleted. They next compared the changes in mitochondrial proteins in wild-type (“normal”) vs NEURL4-deficient cells using mass spectrometry.
According to the researchers, this approach led to the identification of a number of mitochondrial proteins as NEURL4 targets, including mitochondrial LIG3, a protein involved in the repair of damaged mitochondrial DNA, and confirmed that NEURL4 activity is required for mitochondrial DNA (mtDNA) integrity maintenance.
While this research has no obvious clinical implications, the researchers believe it is a significant step toward understanding how cells maintain homeostasis and adapt to oxidative stress.
Mitochondria are membrane-bound organelles with two distinct membranes. And for an intercellular organelle, that’s extremely remarkable. Those membranes serve mitochondria’s primary function, which is to produce energy.
“While this will not directly improve people’s quality of life, we hope it will provide fertile grounds for new translational applications for the treatment of diseases with a mitochondrial component, such as cancer, diabetes, age-related neurodegenerative disorders, and rare mitochondrial diseases,” said co-corresponding author Valentina Perissi, Ph.D., associate professor of biochemistry and co-director of the Boston Nutrition Obesity Research Center at BUSM.
Future study into how NEURL4-mediated changes of certain mitochondrial proteins alter mitochondrial functioning, according to the researchers, could lead to the discovery of novel regulatory techniques to target for therapeutic purposes. A greater understanding of NEURL4 biology could potentially help with male infertility treatment.
Reduced NEURL4 expression in mice is associated with increased mtDNA deletions and markers of male infertility, such as reduced sperm count and increased sperm clumping, according to this study. Mitochondrial DNA deletions have been linked to reduced sperm mobility and infertility in both mice and humans.
The BU Center for Network Systems Biology (CNSB) cooperated on this study with Andrew Emili, Ph.D., and Julian Kwan, Ph.D.
Funding for this study was provided by the National Institutes of Health (R01DK100422 and R01GM127625) to VP; Pilot and Feasibility Award to MDC from the Boston Nutrition and Obesity Center P30DK046200), and by the Grunebaum Cancer Foundation Fellowship to MDC.