High blood glucose levels are to blame for a number of issues in both type 1 and type 2 diabetes. Researchers from Sweden’s Karolinska Institutet discovered a new anti-diabetic chemical that protects the activity of insulin-producing beta cells and avoids excessive blood glucose levels in mice. The findings have been published in the journal Science Translational Medicine.
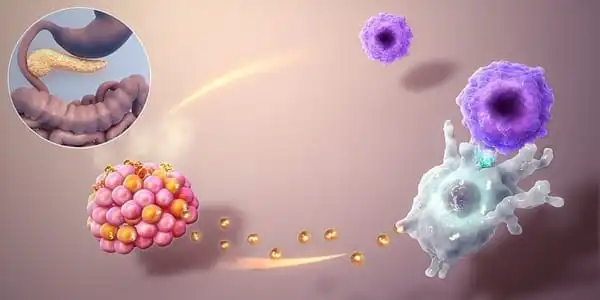
Researchers have revealed that type 1 diabetes individuals can regain their ability to generate insulin. They demonstrated that insulin-producing cells can regenerate outside of the body. Type 1 diabetes is a dangerous condition that affects a large number of children and adolescents. The pancreas stops generating insulin, a hormone that regulates blood sugar levels, as a result of the condition.
When blood sugar levels rise too high, the tiniest blood vessels in the body are destroyed. This can lead to major health issues in the future, such as heart attacks, strokes, blindness, kidney failure, and foot amputations.
Despite the fact that multiple families of glucose-lowering medications are being utilized in diabetes therapy, none of them can stop or reverse the disease’s progression. It is critical to maintain appropriate beta-cell function in order to prevent the advancement of type 1 and type 2 diabetes.
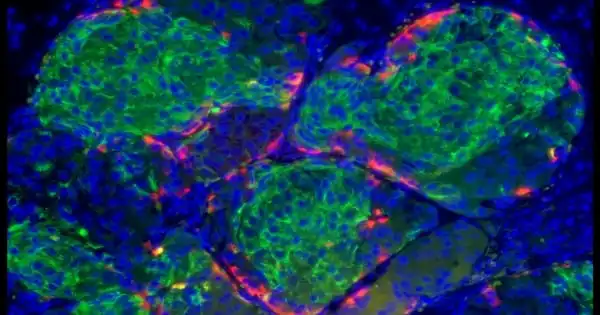
“Beta cells are challenged to create substantial amounts of insulin in diabetes,” explains the study’s first author, Erwin Ilegems, senior researcher at Karolinska Institutet’s Department of Molecular Medicine and Surgery. “According to our findings, this results in a hypoxic state that raises the amounts of HIF-1alpha protein, which lowers beta cell activity. We were able to lower blood glucose levels in diabetic mice by using the HIF-1alpha inhibitor PX-478.”
Beta cells are challenged to create substantial amounts of insulin in diabetes. According to our findings, this results in a hypoxic state that raises the amounts of HIF-1alpha protein, which lowers beta cell activity. We were able to lower blood glucose levels in diabetic mice by using the HIF-1alpha inhibitor PX-478.
Erwin Ilegems
Repurposing an anti-cancer drug
HIF-1alpha (hypoxia-inducible factor-1alpha) governs hypoxia response. HIF-1alpha was given the Nobel Prize in Physiology or Medicine in 2019 for its discovery, and this protein is involved in a variety of disorders. PX-478, an HIF-1alpha inhibitor, has already been studied as an anticancer medication in phase I clinical trials and was well tolerated in these patients.
The scientists were able to demonstrate that the antidiabetic effect of PX-478 was mostly attributable to increased pancreatic beta-cell activity in collaboration with Professor Jorge Ruas’ research group at Karolinska Institutet’s Department of Physiology and Pharmacology.
“We discovered that the insulin-producing cells still had the ability to create insulin when activated in the lab,” Lars Krogvold explains. But what’s unique is that after a few days outside the body, the cells boosted their ability to make insulin. Indeed, some cells became roughly as good at producing insulin as cells from persons who did not have diabetes. When triggered by sugar, some of the pancreas’ hormone-producing cells, known as beta cells, create insulin. Previous research has revealed that when you are diagnosed with type 1 diabetes, you do not immediately lose your ability to generate insulin.”
Because it is generally recognized that insulin production diminishes as diabetes progresses, treatment methods have thus far primarily focused on increasing beta-cell insulin production. However, this strategy has not been as successful as anticipated.
“Current medicines targeting beta cells have only a temporary favorable effect on insulin secretion,” says Per-Olof Berggren, professor of Karolinska Institutet’s Department of Molecular Medicine and Surgery. “Over time, these medicines cause beta-cell depletion.”
Long-term treatment of diabetes
PX-478, unlike other therapies, improves beta-cell function without increasing insulin secretion. As a result, the researchers believe it can avoid beta cell fatigue and hence be more effective in the long-term therapy of diabetes.
“We are now planning to further investigate the translatability of our findings in order to hopefully pave the way for future clinical trials,” says Teresa Pereira, co-last author of the study and researcher at Uppsala University’s Department of Medical Cell Biology (formerly employed by Karolinska Institutet). “We will begin by using ‘humanized’ diabetic mice to investigate the effect of PX-478 on human pancreatic beta-cell function.”
“If we can find a mechanism to arrest the illness process, our findings may imply that insulin production can be partially restored.” Insulin production has a bigger capacity than previously realized. Those who can maintain a specific amount of insulin production have a lesser risk of acquiring health problems later in life. “If you need less supplemental insulin, you’ll be better off as a patient,” adds Krogvold.