Chimeric antigen receptor (CAR) T-cell therapy has transformed the treatment of blood malignancies such as leukemias, lymphomas, and multiple myeloma. However, Black and Hispanic patients were largely absent from the key clinical trials that led to CAR T-cell therapy approval by the US Food and Drug Administration. Thakkar et al. reported in the journal Bone Marrow Transplantation that Black and Hispanic patients had equivalent outcomes and side effects following CAR T-cell therapy to their White and Asian counterparts.
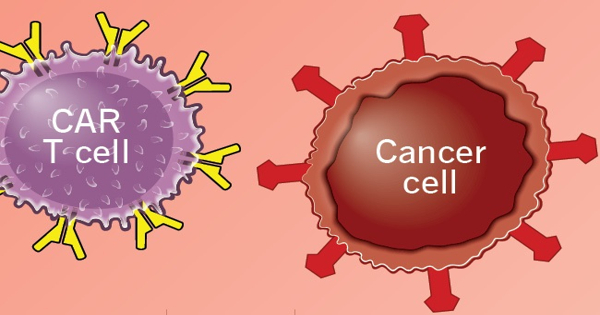
CAR-T therapy, a type of immunotherapy that stimulates T-cells to target and destroy cancer cells, has transformed the treatment of blood cancers such as leukemias, lymphomas, and, most recently, multiple myeloma. However, Black and Hispanic people were mostly absent from the key clinical trials that led to CAR-T cell therapy approval by the US Food and Drug Administration.
People who identify as Black or Hispanic frequently have tumor biology, immune system biology, and side effects that are not shared by White people. However, only a small number of minorities were enrolled in the key trials that led to the FDA’s approval of CAR T-cell therapy.
In a study published in Blood Marrow Transplantation (BMT), investigators at the National Cancer Institute-designated Montefiore Einstein Cancer Center (MECC) report that Black and Hispanic patients had outcomes and side effects following CAR-T treatment that were comparable to their white and Asian counterparts.
Our findings show that we can effectively treat people from historically marginalized groups with CAR-T; our hope is that more people from a diverse range of racial and ethnic backgrounds will be included in clinical trials.
Amit Verma
“Representation in cancer clinical trials is critical to ensuring that treatments are safe and effective for everyone,” said Mendel Goldfinger, M.D., co-corresponding author of the paper, a medical oncologist at Montefiore Health System, assistant professor of medicine at Albert Einstein College of Medicine, and member of the MECC Cancer Therapeutics Program. “We were overjoyed to learn that our patients who identify as Black or Hispanic receive the same benefits from CAR-T therapy as white patients. We can only begin to argue that cancer treatment is transformative when these technologies benefit everyone who comes to us for care.”
People who identify as Black and Hispanic often have tumor biology, immune system biology, and side effects that are distinct from white people. However, very few minorities were enrolled in the major trials that led the FDA to approve CAR-T cell therapy.
Parity for Black and Hispanic Patients
The latest BMT study looked at the results of 46 patients who were treated at Montefiore between 2015 and 2021. Seventeen participants were Hispanic, nine were African American, fifteen were Caucasian, and five were Asian.
After treatment, 58 percent of Black and Hispanic patients had a complete reaction, while 19 percent had a partial response. There were no statistical variations in racial and ethnic backgrounds among white and Asian patients, with 70% achieving a complete response and 20% achieving a partial response. When it came to serious adverse effects, the results were similar: Approximately 95% of individuals in each group experienced mild to moderate cytokine release syndrome, a typical adverse effect of immunotherapy that causes fever and other flu-like symptoms.
CAR T-cell treatment entails collecting white blood cells from a cancer patient and reprogramming the T cells — the wandering warriors of the immune system — with an antibody-like protein known as Chimeric Antigen Receptor, or CAR. The changed cells are returned to the patient’s body in less than 10 minutes. These re-engineered T cells skip healthy cells and grab on to and kill malignant cells, thus fighting cancer with a patient’s own immune system.
Diversifying Cancer Clinical Trials
“Our findings show that we can effectively treat people from historically marginalized groups with CAR-T; our hope is that more people from a diverse range of racial and ethnic backgrounds will be included in clinical trials,” said co-author Amit Verma, M.B.B.S., associate director of translational science at MECC, director of the division of hemato-oncology at Montefiore and Einstein, and professor of medicine and developmental and molecular biology Ira Braunschweig, M.D., an associate professor of medicine at Einstein and the director of Stem Cell Transplantation and Cellular Therapy, as well as the clinical program director for Hematologic Malignancies at Montefiore, is a co-corresponding author on the paper.
Minorities make up nearly 80 percent of clinical trial participants at Montefiore, compared to only 8 percent nationally.
“It is not enough for us as an academic medical institution to make innovative therapies like CAR-T available,” said Susan Green-Lorenzen, R.N., M.S.N., Montefiore’s system senior vice president of operations and study co-author. “We must be at the forefront of ensuring that these treatments are effective for the communities we serve, and this research underscores that dedication.”