The human papilloma virus (HPV) is the name specified to a family of viruses. Diverse types of HPV are classed as either high risk or low risk, depending on the conditions they can cause. For example, some types of HPV can cause warts or verrucas. Other types are connected with cervical cancer.
In 99% of cases, cervical cancer occurs as a result of a history of infection with high-risk types of HPV. Often, infection with the HPV causes no symptoms.
Importance of HPV vaccine?
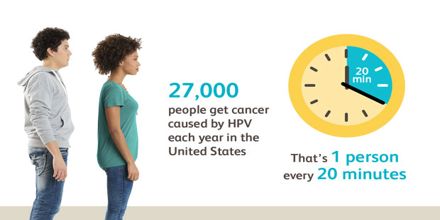
HPV vaccine is significant because it protects against cancers caused by human papilloma virus (HPV) infection. HPV is a very familiar virus; nearly 80 million people—about one in four—are currently infected in the United States. About 14 million people, including teens, become infected with HPV each year.
Most people with HPV never grow symptoms or health problems. Most HPV infections (9 out of 10) go away by themselves within two years. But, sometimes, HPV infections will last longer, and can reason definite cancers and other diseases. HPV infection can cause:
- cancers of the cervix, vagina, and vulva in women;
- cancers of the penis in men; and
- cancers of the anus and back of the throat, including the base of the tongue and tonsils (oropharynx), in both women and men.
Every year in the United States, HPV causes 30,700 cancers in men and women. HPV vaccination can prevent most of the cancers (about 28,000) from occurring.

Different types of HPV
There are over 100 different types of HPV, with around 40 types that involve the genital area.
Infection with some high-risk types of HPV can cause abnormal tissue increase as well as other cell changes that can lead to cervical cancer.
Infection with other types of HPV may cause:
- genital warts: small growths or skin changes on or around the genital or anal area, these are the most common viral sexually transmitted infection (STI) in the UK
- skin warts and verrucas
- vaginal cancer or vulval cancer (although these types of cancer are rare)
- anal cancer or cancer of the penis
- some cancers of the head and neck
- laryngeal papillomas (warts on the voice box or vocal cords)

How the HPV vaccine helps
A vaccine called Gardasil is used in the national NHS cervical cancer vaccination programme. Gardasil protects against the two types of HPV, between them responsible for more than 70% of cervical cancers in the UK.
A bonus of using Gardasil to prevent cervical cancer is that it prevents genital warts too.
Why is the HPV vaccine given at such a young age?
The HPV virus is very common and is easily spread by sexual activity.
As much as half the population will be infected at some time in their life. In most cases, the virus doesn’t do any harm because your immune system gets rid of the infection. But in some cases, the infection persists and can lead to health problems.
Although most girls don’t start having sex until after they’re 16 years of age, it’s important that they are protected against HPV infection early enough and a good time is in the early teenage years. Getting the vaccine as early as possible will protect them in the future.
How is the HPV vaccine given?
The HPV vaccine is at present given as a series of two injections within a six- to 24-month period. Girls who began their course of HPV vaccination before September 2014 receive three injections.
Who else should get the HPV vaccine?
Teen boys and girls who did not start or finish the HPV vaccine series when they were younger should get it now.
HPV vaccine is recommended for young women through age 26, and young men through age 21. HPV vaccine is also recommended for the following people, if they did not get vaccinated when they were younger:
- young men who have sex with men, including young men who identify as gay or bisexual or who intend to have sex with men through age 26;
- young adults who are transgender through age 26; and
- young adults with certain immunocompromising conditions (including HIV) through age 26.