Neurons in the preoptic hypothalamus, the region of the brain that regulates sleep and body temperature, are rhythmically activated during non-rapid eye movement sleep (NREM), according to new research. According to new research from the University of Pennsylvania’s Perelman School of Medicine, stress activates these brain cells out of turn, causing “microarousals” that disrupt sleep cycles and shorten the duration of sleep episodes.
While our bodies are at rest when we sleep, our brains remain very active throughout the four stages of sleep. There are three stages of NREM sleep and one stage of rapid eye movement (REM) sleep in each 90-minute sleep cycle. Brain waves, heartbeat, and breathing all slow down during the first two stages of NREM sleep, as does body temperature. Spindles and K-complexes, which are short bursts of activity responsible for processing outside stimuli as well as consolidating memory, are also included in stage two.
The third stage of the NREM sleep cycle is when the body releases growth hormone, which is necessary for body repair, immune system health, and memory enhancement. Brain waves, known as delta waves, are larger during phase three. Memory formation, emotional processing, and brain development all depend on REM sleep, which occurs during this phase when dreaming normally occurs.
When you have a bad night of sleep, you notice that your memory isn’t as good as it normally is, or your emotions are all over the place – but a bad night of sleep interrupts so many other processes throughout your body. This is even more heightened in individuals with stress-related sleep disorders.
Shinjae Chung
“When you have a bad night of sleep, you notice that your memory isn’t as good as it normally is, or your emotions are all over the place – but a bad night of sleep interrupts so many other processes throughout your body. This is even more heightened in individuals with stress-related sleep disorders,” said senior author, Shinjae Chung, PhD, an assistant professor of Neuroscience. “It’s crucial to understand the biology driving the brain activity in these crucial stages of sleep, and how stimuli like stress can disrupt it, so that we might someday develop therapies to help individuals have more restful sleep that allows their brain to complete these important processes.”
The researchers monitored the activity in the preoptic area (POA) of the hypothalamus of mice during their natural sleep and found that glutamatergic neurons (VGLUT2) are rhythmically activated during NREM sleep. They also found that VGLUT2 neurons were most active during wakefulness, and less active during NREM and REM sleep.
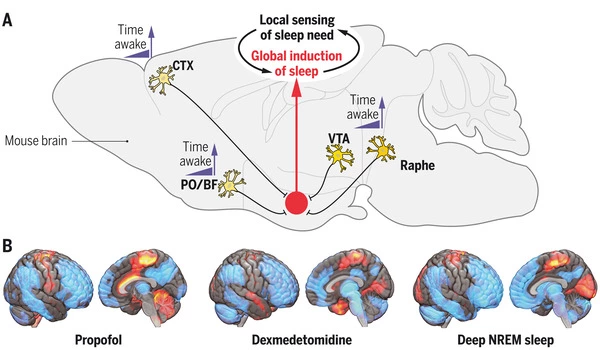
VGLUT2 neurons were the only active neurons within the POA during microarousals in NREM sleep, and their signals began to increase in the time before a microarousal. To confirm that active VGLUT2 neurons were indeed the cause of microarousal, the researchers stimulated VGLUT2 neurons in sleeping subjects, which increased the number of microarousals and wakefulness immediately.
The researchers then exposed subjects to a stressor, which increased awake time and microarousals while decreasing overall time spent in REM and NREM sleep, to demonstrate the link between stress and increased VGLUT2 neuron activation. Researchers also discovered increased VGLUT2 neuron activity in stressed subjects during NREM sleep. Furthermore, when researchers inhibited VGLUT 2 neurons, microarousals during NREM sleep were reduced and NREM sleep episodes were lengthened.
“The glutamatergic neurons in the hypothalamus give us a promising target for developing treatments for stress-related sleep disorders,” said Jennifer Smith, a graduate researcher in Chung’s lab. “Being able to reduce interruptions during the important stages of non-REM sleep by suppressing VGLUT2 activity would be groundbreaking for individuals struggling with disrupted sleep from disorders like insomnia or PTSD.”