Inflammation indicates that our body is protecting itself against an attack. However, when this response becomes excessive, such as in the brain, it can result in catastrophic neurological or mental illnesses. A group of researchers from the University Of Geneva (UNIGE), the University Hospitals of Geneva (HUG), Imperial College London, and Amsterdam UMC explored a marker protein used in medical imaging to visualize cerebral inflammation but its meaning was still unknown.
The researchers discovered that a high concentration of this protein is associated with a high concentration of inflammatory cells, but its presence does not indicate that these cells are overactive. These findings, which were published in Nature Communications, pave the way for better observation of neuroinflammatory processes as well as a re-reading of earlier research on the issue.
Inflammation is a natural defensive reaction that the immune system initiates. It lets our cells defend themselves against aggression, such as injury or infection. However, this response might spiral out of control, resulting in the onset of significant diseases. This overactivation can play a role in the mechanisms of neurodegenerative diseases (Alzheimer’s, amyotrophic lateral sclerosis, multiple sclerosis) and psychiatric diseases (schizophrenia, bipolar disorder, depression) when it occurs in the brain, which is known as neuroinflammation.
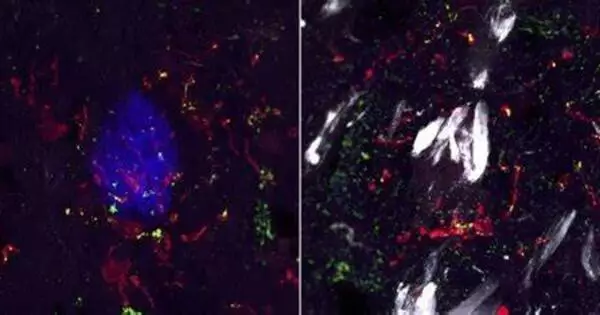
Microglial cells in the brain play a crucial role in inflammation and its possible overactivation. When they are ”activated,” they can phagocytize diseased cells or proteins and even create protective chemicals. Currently, only one marker can be utilized in medical imaging to find and measure microglia non-invasively and in vivo: the TSPO protein, which is found in these cells. Positron Emission Tomography (PET), a standard imaging tool, can detect this protein.
These findings contribute to a better understanding of the role of microglia in neuroinflammation. They will aid in optimizing the focus of future investigations as well as reviewing the findings of prior research.
Stergios Tsartsalis
What does TSPO protein reveal?
”Hundreds of research have employed this protein’s PET scans to investigate and quantify microglia. ”However, no study has succeeded in properly defining the importance of its quantity in the setting of an inflammatory reaction,” says Stergios Tsartsalis, senior clinical associate at the UNIGE Faculty of Medicine’s Department of Psychiatry. Is a high level of TSPO associated with a high level of inflammatory cells?
Is this a symptom of their hyperactivity? Stergios Tsartsalis and members of Prof Philippe Millet’s team from the HUG’s Laboratory of Translational Imaging in Psychiatric Neuroscience and the UNIGE’s Group of Molecular Neuroimaging in Psychiatry set out to find out with researchers from Imperial College London (Dr David Owen) and Amsterdam UMC (Prof Sandra Amor).
The multinational team studied the brains of mice models of Alzheimer’s disease, amyotrophic lateral sclerosis, and multiple sclerosis, as well as post-mortem brain samples from humans suffering from the same disorders. ”We determined that a high density of TSPO protein indicates a high density of microglia. The observation of TSPO, on the other hand, does not allow us to say whether or not the inflammatory cells are overactivated,” says the UNIGE researcher and co-first author of the study.

Re-reading the past, optimizing the future
Decoding a signal for brain inflammation would be a tremendous leap in neuroscience, with considerable implications for the diagnosis and treatment of many neurological diseases.
This study emphasizes the importance of TSPO medical imaging: it allows researchers to detect cases where the neuroinflammatory disease is associated with a decrease in the number of glial cells. Furthermore, the researchers discovered two indicators of microglia activity in humans, the LCP2 and TFEC proteins, which pave the path for new diagnostic imaging methods.
”These findings contribute to a better understanding of the role of microglia in neuroinflammation. They will aid in optimizing the focus of future investigations as well as reviewing the findings of prior research,” says Stergios Tsartsalis. This study, supported by the Swiss National Science Foundation and the Prof Dr Max Clotta Foundation, sets the stage for effective observation of the immune mechanisms of neurological and psychiatric diseases within the two Geneva institutions and beyond.