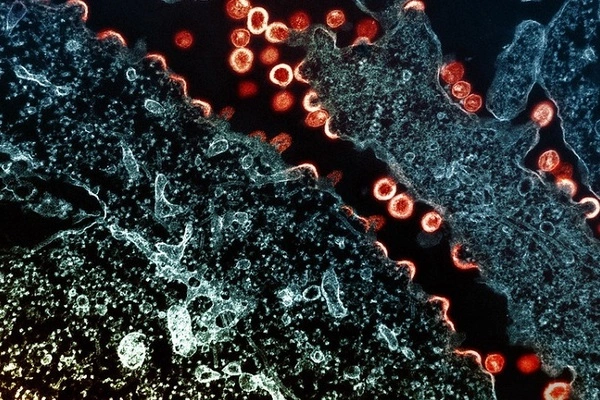
HIV reservoirs are groups of infected cells that harbor the virus and are able to survive and replicate despite antiretroviral therapy (ART). These reservoirs are a major obstacle to curing HIV because they can reactivate the virus and cause disease even after long-term suppression of viral replication by ART.
A team of researchers discovered that HIV can form reservoirs where it can hide and persist during antiretroviral therapy as early as the first days of infection. For the first time in humans, a research team discovered that HIV can form reservoirs in which it can hide and persist during antiretroviral therapy as early as the first days of infection. Until now, scientists did not know when or how these viral reservoirs, the presence of which is a major impediment to curing HIV, are established in humans.
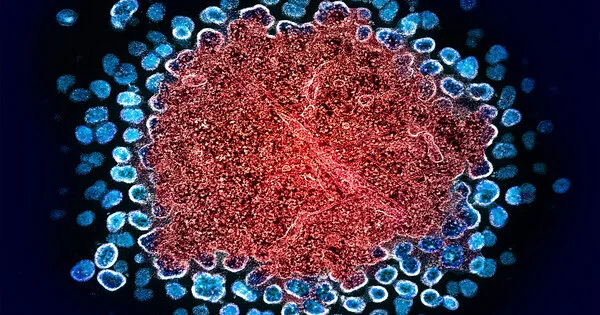
Scientists led by Nicolas Chomont, a researcher at the CHUM Research Center (CRCHUM) and professor at Université de Montréal, discovered in a study published in the journal Immunity that a small fraction of the virus integrates into the genome of CD4+ T cells in the first weeks of infection (the acute phase), but does not replicate there. As a result, it escapes the detection of the fastest diagnostic tool available, which detects active viral replication. HIV’s primary target cells are CD4+ T cells. They are white blood cells that activate the human body’s defense against infection.
We succeeded in detecting the presence of the virus through sequencing even when it was hidden in cells that weren’t participating in viral replication.
Nicolas Chomont
“With the help of an analysis technique developed in our laboratory, we were able to observe and count the T cells infected by the virus in human samples collected in the earliest stages of the infection,” said Chomont, the study’s principal author. “We succeeded in detecting the presence of the virus through sequencing even when it was hidden in cells that weren’t participating in viral replication.”
Pierre Gantner, a former postdoctoral student in Chomont’s lab and the study’s first author, had access to blood and inguinal lymph node tissue samples from 25 people in the first acute-infection cohort of the US Military HIV Research Program in Thailand to study these early stages of the virus’s spread.
RV254/SEARCH010 is a cohort that began more than ten years ago in collaboration with the Thai Red Cross AIDS Research Centre and has enrolled nearly 800 volunteers. Chomont and his team have been working closely with their colleagues in Thailand since the company’s inception.
Mapping the types of infected cells
The CRCHUM researchers were able to count the CD4+ T cells infected by the virus during the acute phase of the infection using their analysis technique. In less than seven days, the number of infected cells increased from 10 to 1,000 per million CD4+ T cells, demonstrating the extreme speed with which HIV spreads.
The researchers also discovered that the characteristics of HIV-targeted cells changed quickly and differed depending on whether they were found in the blood or lymph nodes during the first weeks of infection.
“For example, we noticed that few Tfh – T follicular helper cells – are infected by the virus during the acute phase of the infection,” said Chomont. “Since they play a crucial role in viral replication, the scientific community thought that they were the first to be infected. In fact, we counted a lot more [infected Tfh] during the chronic phase of the disease, which is about two months after infection. At that point, they are actively contributing to the development of the disease.”
Until now, these types of studies have been carried out on animal models. Therefore, this is the first time that the early stages of the infection in humans have been described so precisely.
Destabilizing the reservoirs
A large part of global research dedicated to the study of HIV focuses on how to reactivate the virus lying dormant in the reservoirs in order to neutralize it.
“‘The earlier we start antiretroviral therapy, the more we prevent the virus from replicating and the smaller the reservoirs become. We demonstrated this in 2020 “Chomont stated. “However, it appears clear that early antiretroviral therapy should be combined with another treatment to force the virus out of its hiding places, because latent reservoirs will have already been established in people infected with HIV at the time of diagnosis.”
Chomont’s research team is currently evaluating whether this type of treatment administered during the acute infection phase would prevent the establishment of viral reservoirs in collaboration with scientists from the United States.