Antimicrobial resistance is a critical and developing global issue. Researchers are looking into phages, viruses that infect bacteria, as a potential cure. In a recent study, researchers successfully changed DNA from four different types of phages to eradicate a dangerous infection. The technique can also be utilized to generate more phage varieties for further investigation.
Northwestern University researchers successfully induced a deadly disease to destroy itself from the inside out.
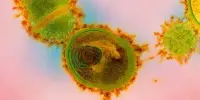
In the latest work, researchers changed DNA from a bacteriophage, or “phage,” which is a type of virus that infects and replicates inside bacteria. The DNA was then inserted into Pseudomonas aeruginosa (P. aeruginosa), a dangerous bacterium that is also antibiotic-resistant. Once within the bacterium, the DNA overcame the pathogen’s defense mechanisms, forming virions that slashed through the bacterium’s cell and killed it.
The experimental effort, which builds on a rising interest in “phage therapies,” is an important step toward creating designer viruses as new medications to fight antibiotic-resistant bacteria. It also exposes important details about the inner workings of phages, a little-studied field of biology.
The study was published in the journal Microbiology Spectrum.
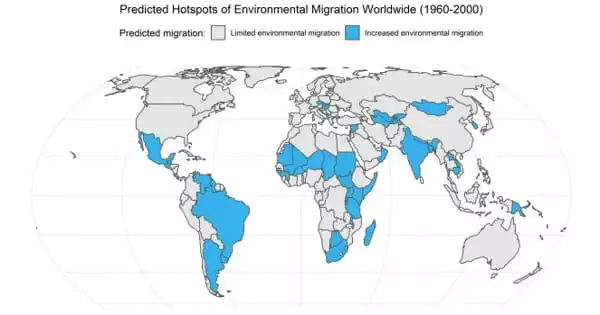
Antimicrobial resistance is sometimes referred to as the ‘silent pandemic. The numbers of infections and deaths from infections are increasing worldwide. It’s a massive problem. Phage therapy has emerged as an untapped alternative to our reliance on using antimicrobials.
Erica Hartmann
“Antimicrobial resistance is sometimes referred to as the ‘silent pandemic,'” said Northwestern’s Erica Hartmann, who led the work. “The numbers of infections and deaths from infections are increasing worldwide. It’s a massive problem. Phage therapy has emerged as an untapped alternative to our reliance on using antimicrobials. But, in many ways, phages are microbiology’s ‘final frontier.’ We don’t know much about them. The more we can learn about how phage work, the more likely we can engineer more effective therapeutics. Our project is cutting-edge in that we are learning about phage biology in real time as we engineer them.”
An indoor microbiologist, Hartmann is an associate professor of civil and environmental engineering at Northwestern’s McCormick School of Engineering and a member of the Center for Synthetic Biology.
Desperate need for antibiotic alternatives
The growth of antibiotic resistance, which is linked to increased antimicrobial use, is an urgent and growing hazard to the global population. According to the Centers for Disease Control and Prevention (CDC), about 3 million antimicrobial-resistant infections occur each year in the United States, resulting in the deaths of over 35,000 people.
The mounting dilemma has prompted experts to seek alternatives to antibiotics, which are rapidly losing potency. In recent years, researchers have begun to investigate phage therapy. Even though there are billions of phages, scientists know very little about them.
“For every bacterium that exists, there are dozens of phages,” Hartmann said. “So, there is an astronomically large number of phages on Earth, but we only understand a handful of them. We haven’t necessarily had the motivation to really study them. Now, the motivation is there, and we are increasing the number of tools we have to dedicate to their study.”

Treatment without side effects
To investigate possible phage therapeutics, researchers either identify or adapt an existing virus to selectively target a bacterial illness while without disturbing the rest of the body. Ideally, scientists may one day adapt a phage therapy to infect a specific bacterium and create “a la carte” treatments with specific qualities and properties to cure individual infections.
“What’s powerful about phage is it can be very specific in the way that antibiotics are not,” Hartman said. “Taking an antibiotic to treat a sinus infection, for example, affects your entire gastrointestinal tract. A phage therapy can be tailored to target only the illness.
While other researchers have investigated phages therapies, almost all of those studied have focused on using phages to infect Escherichia coli. Hartmann, however, decided to focus on P. aeruginosa, one of the five most deadly human pathogens. Particularly dangerous for people with compromised immune systems, P. aeruginosa is a leading cause of hospital infections, often infecting patients with burn or surgery wounds as well as lungs in people with cystic fibrosis.
“It is one of the highest priority, multi-drug resistant pathogens that many people are really concerned about,” Hartmann said. “It is extremely drug resistant, so there is an urgent need to develop alternative therapeutics for it.”
Mimicking infection, bypassing defenses
In the work, Hartmann and her colleagues began with P. aeruginosa bacteria and extracted DNA from multiple phage species. Then they utilized electroporation, a technique that uses short, high-voltage electrical pulses, to create temporary holes in the bacteria’s outer cell. Phage DNA infiltrated the bacteria through these perforations, mimicking the infection process.
In some cases, the bacterium identified the DNA as a foreign thing and destroyed it to protect itself. However, after optimizing the technique with synthetic biology, Hartmann’s team was able to eliminate the bacteria’s antiviral self-defense systems. In some circumstances, the DNA effectively transported information into the cell, producing virions that killed the bacterium.
“Where we were successful, you can see dark spots on the bacteria,” Hartmann said. “This is where the viruses burst out of the cells and killed all the bacteria.”
After this success, Hartmann’s team introduced DNA from two more phages that are naturally unable to infect their strain of P. aeruginosa. Yet again, the process worked.
Phage manufacturing in a cell
Not only did the phage destroy the bacterium, but the bacteria also discharged billions of additional phages. These phages can then be employed to eliminate other bacteria, such as those that are causing an infection. Hartmann intends to continue manipulating phage DNA to improve possible medicines. Her team is currently examining the phages released by P. aeruginosa.
“This is an important piece in making phage therapies,” she went on to say. “We can study our phage in order to decide which ones to develop and eventually mass produce them as a therapeutic.”
The Walder Foundation, the National Science Foundation, and the National Institutes of Health funded the study, “A synthetic biology approach to assemble and reboot clinically relevant Pseudomonas aeruginosa tailed phages,”