Two separate brain networks have been found to be connected with higher and decreased depression symptoms in a recent study that ties the site of brain injury to depression levels in individuals after the injury.
These brain networks may be prospective targets for neuromodulation therapies to treat depression, according to the extensive study conducted by scientists with University of Iowa Health Care.
Deep brain stimulation and other neuromodulation technologies are developing as cutting-edge non-pharmacological treatments for mood disorders. However, there is currently a lack of knowledge regarding the optimum brain regions to focus on for therapeutic purposes.
The latest research, which was reported in the journal Brain, employed depression scores and brain imaging scans from 526 individuals who had had localized brain damage as a result of a stroke or another type of traumatic brain injury.
The locations of the brain lesions and the patients’ levels of depression in the months after the brain injury were linked by the researchers through a thorough statistical analysis of the patient data.
“We found some really interesting results identifying specific brain structures that were associated with higher levels of depression post lesion, and surprisingly, also found some areas that were associated with lower-than-average levels of depression post lesion.” says Nicholas Trapp, MD, UI assistant professor of psychiatry and lead author of the study.
Being able to identify these brain regions is really a product of having a large sample to study. It’s very challenging to recruit these patients and collect the data that’s required. The decades of efforts here at the University of Iowa (establishing and maintaining the Iowa Neurological Patient Registry) positions us extremely well to do these types of studies.
Nicholas Trapp
Risk and resilience networks in depression
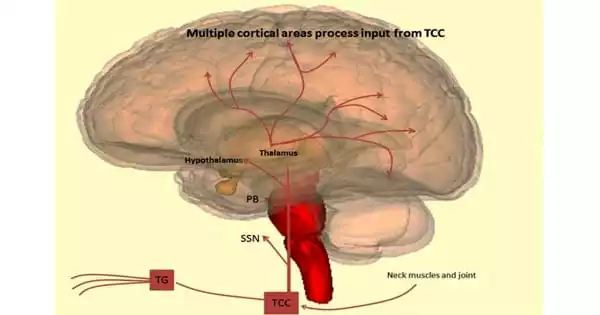
The researchers then found that the risk and resilience regions were not dispersed randomly throughout the brain using information from functional brain scans of healthy patients to comprehend how these structures were interconnected.
Instead, areas most significantly linked to greater depression were found to be near the nodes of the so-called salience network, which is involved in emotion processing, task reorientation, and attention.
In contrast, the default mode network, which is assumed to be involved in introspection or self-referential thinking, was part of the peak resilience regions that were linked to lower levels of depression.
“Previous studies have suggested nodes of this network may be hyperactive in people with depression, who are prone to ruminating,” says Trapp, who also is a member of the Iowa Neuroscience Institute. “It’s possible that lesions within this network may alter that circuit in a way that leads people to report less depression.”
Patients who had brain lesions outside of either network and who served as a comparison group in the study had average depression scores after suffering a brain injury.
Strength in numbers
Trapp and his colleagues’ original lesion mapping method is a potent tool for determining whether a brain region is necessary for a behavior, emotion, or cognitive capacity. If a certain area is damaged and the ability is lost, the area is probably necessary for the ability.
Although earlier smaller studies may have been hampered by the need for data from a large number of patients, it is necessary to find an effect when the areas are dispersed across a network within the brain.
Trapp and his team were able to conduct they study thanks to two large patient registries: the Iowa Neurological Patient Registry based at the UI, and the Vietnam head injury study, which is affiliated with researchers at Northwestern University.
“Being able to identify these brain regions is really a product of having a large sample to study,” Trapp says. “It’s very challenging to recruit these patients and collect the data that’s required. The decades of efforts here at the University of Iowa (establishing and maintaining the Iowa Neurological Patient Registry) positions us extremely well to do these types of studies.”
Potential new targets for neuromodulation
Trapp hopes that the results will advance knowledge of the factors that contribute to depression and possibly result in more effective treatments.
“This could open the doors to potential studies looking at deep brain stimulation, or non-invasive forms of stimulation like TMS, where we might be able to modulate the specific brain areas or networks that we’ve identified, to try to get antidepressant effect, or potentially other therapeutic effects,” he says.
In addition to Trapp, the UI research team included Aaron Boes, Joel Bruss, Kenneth Manzel, and Dan Tranel, of the UI Department of Neurology, and Jordan Grafman of the Shirley Ryan AbilityLab, at Northwestern University Feinberg School of Medicine in Chicago.
The study was funded in part by grants from the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, and the Kiwanis Neuroscience Research Foundation.