A chronic brain disorder called epilepsy is characterized by recurrent seizures. This can develop at any age, but it is more common in children and older adults. The causes of epilepsy can vary, but some common factors include genetics, brain injury, infections, or developmental disorders.
Drug-refractory individuals, or those who do not react to medication, make up about 30% of the epilepsy population. Living with epilepsy can be challenging, but with the proper treatment and support, many people with epilepsy are able to lead normal, active lives.
Temporal lobectomy of the epileptogenic zone can reduce or eliminate symptoms, but not all patients are candidates for surgical resection, and neurological damage following surgery can result in speech or movement paralysis, necessitating the urgent need for a new effective treatment.
Recently, a joint team of researchers from POSTECH and Samsung Medical Center developed a therapeutic modality to treat intractable epilepsy by stimulating the deep part of the brain, personalized to each patient’s individual brain structure. The findings from the study were published in Nature Communications.
Recently, deep brain stimulation (DBS) has been introduced as an alternative to the surgical approach for intractable epilepsy. With the use of the cutting-edge medical technique known as DBS, electrodes are implanted deep into the brain to stimulate the area that causes seizures. It can lessen both the intensity and frequency of seizures by more than 70%.
This study can be applied to the development of more precise and personalized medical devices as a ‘future convergence medical solution research’ in which engineering and medicine converge in the areas related to high-level brain stimulation. It is a highly practical engineering-based medical solution that is clinically applicable thanks to the collaboration with Samsung Medical Center.
Professor Sung-Min Park
However, conventional DBS has failed to reflect individual brain structures and applied stimuli in a uniform manner. As a result, broadly applied stimuli spread beyond the target tissues, evoking pain, increased depression, and other side effects. It also had a disadvantage of shortening battery life.
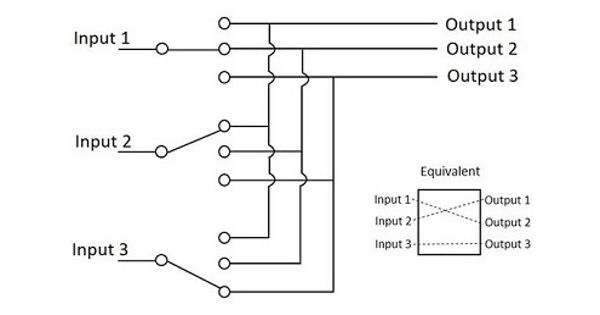
The combined team suggested using sequential narrow-field (SNF) stimulation in a rat model to get around these problems. The hippocampus is big and extended and serves as the primary seizure site in those with temporal lobe epilepsy. The sensors recognize when the hippocampus experiences a seizure and concentrate low-intensity stimulation energy there only.
The SNF stimulation created in this work reliably predicts when seizures will start, promptly reduces symptoms, and solely stimulates the target region of the hippocampus without stimulating nearby brain tissues.
For this, SNF stimulation shows promise to a medical solution that is based on bioelectronic technology that is safer and more effective than the conventional DBS methods, which can be applied to other neurological diseases.
Professor Young-Min Shon (Department of Neurology) who is the director of Biomedical Engineering Research Center at the Samsung Medical Center explained, “This method can be easily applied clinically and promises to become an optimal treatment for intractable epilepsy in the future.”
On the significance of the study, the lead investigator Professor Sung-Min Park commented, “This study can be applied to the development of more precise and personalized medical devices as a ‘future convergence medical solution research’ in which engineering and medicine converge in the areas related to high-level brain stimulation. It is a highly practical engineering-based medical solution that is clinically applicable thanks to the collaboration with Samsung Medical Center.”
This study was supported by the STEAM (Pioneer Research Center) program’s “developing a fully autonomous neural reset system to overcome intractable chronic diseases with brain homeostasis imbalances” project.