Pediatric brain tumors are tumors that originate in the brain or spinal cord of children, typically under the age of 18. These tumors can be either benign (non-cancerous) or malignant (cancerous), and they can occur in different parts of the brain, such as the cerebellum, brain stem, or cerebral hemispheres.
Researchers from Memorial Sloan Kettering Cancer Center and Mount Sinai Health System have created a new drug delivery method that makes use of nanoparticles to deliver anti-cancer medications more precisely and successfully to treat pediatric brain tumors.
The method enables improved delivery of anti-cancer medications to the precise sites of brain tumors while conserving healthy brain tissue. Their study, which was released on March 2, 2023 in Nature Materials, found that the outcome was an improvement in the efficacy and a decrease in the toxicities of anti-cancer medications.
“We show that we can more successfully deliver lower doses of the drug in a more effective manner to the specific sites of tumor within the brain, while sparing the bone toxicity that is seen in younger patients,” says Praveen Raju, MD, Ph.D., Co-Director of the Children’s Brain and Spinal Tumor Center at Mount Sinai Kravis Children’s Hospital, and senior author of the study.
The prognosis for pediatric brain tumors varies depending on the type and grade of the tumor, as well as the child’s age and overall health. Some tumors may be successfully treated, while others may be more difficult to treat or may recur despite treatment. Close monitoring and ongoing care are often needed to manage any long-term effects of treatment and to monitor for recurrence.
In addition, we showed that this targeted drug delivery approach is further enhanced with very-low-dose radiation, which is a standard therapy already used for most children and adults with primary and metastatic brain tumors.
Dr. Raju
Medulloblastoma is the most common malignant pediatric brain tumor, accounting for about 20% of all brain tumors in children. Around 30% of people have it, which is very aggressive, challenging to cure, and considered incurable. Even “cured” youngsters endure serious long-term health problems and disabilities, mostly as a result of the harmful side effects of radiation and chemotherapy.
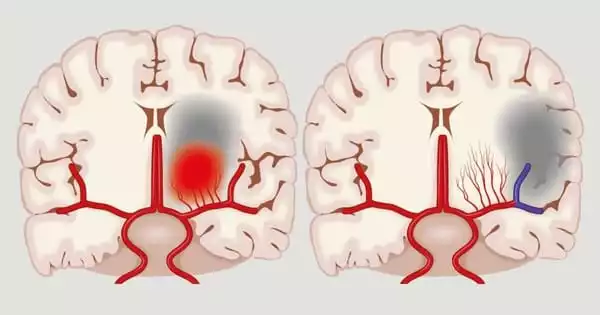
A separate and tightly regulated blood-brain barrier, which typically shields the brain from infections or other hazardous chemicals, prevents site-directed medicine delivery to the afflicted brain tissue.
The immune system often uses a technique to direct white blood cells to areas of infection, inflammation, or tissue damage, and the researchers used this process in this investigation. Immune cells can exploit the homing mechanism on active blood arteries to travel to the areas of the body where they are most required instead of randomly distributing throughout the body.
The scientists were able to direct their drug-loaded nanoparticles to the disease site and away from healthy brain regions by using this special homing trait, which is also present in the blood arteries of brain tumors.
The research team was able to improve the effectiveness of an anti-cancer drug that might be useful for a subset of medulloblastoma patients but is currently constrained by the bone toxicity it secondarily causes in children by using the new drug delivery platform in a genetically relevant mouse model of the disease.
“In addition, we showed that this targeted drug delivery approach is further enhanced with very-low-dose radiation, which is a standard therapy already used for most children and adults with primary and metastatic brain tumors,” says Dr. Raju, Associate Professor of Neurology, Neuroscience, and Pediatrics at Icahn School of Medicine at Mount Sinai.
“Importantly, our blood-brain barrier drug delivery approach has the potential to improve the delivery of drugs for other pediatric brain tumors and localized diseases in the brain in both children and adults, including focal epilepsy, multiple sclerosis, stroke, and possibly neurodegenerative disorders.”
“Certain proteins appear on blood vessels at sites of inflammation that help white blood cells exit the bloodstream. They work like police officers at the site of a car accident, who let in emergency personnel to help,” says Daniel Heller, Ph.D., Head of the Cancer Nanomedicine Laboratory and Member in the Molecular Pharmacology Program at Memorial Sloan Kettering Cancer Center, and senior author on the study. “We sent in our own emergency personnel, in the form of drug-loaded nanoparticles, composed of certain sugar molecules that can target these same proteins.”
The effectiveness of various classes of authorized and experimental therapies is expected to be improved with further study and development of this technique to harness and enhance the transport of materials through the blood-brain barrier and other places.
This drug delivery platform can be utilized to treat various inflammatory disorders that affect the central nervous system and other parts of the body, as well as tumors that affect the brain and other parts of the body.