Cirrhosis
Definition: Cirrhosis is a serious degenerative disease that occurs when healthy cells in the liver are damaged and replaced by scar tissue, usually as a result of alcohol abuse or chronic hepatitis. The word cirrhosis is from Greek: κίρρωσις; kirrhos κιρρός “yellowish” and -osis (-ωσις) meaning “condition”, describing the appearance of a cirrhotic liver. It is a progressive disease, developing slowly over many years. If it is allowed to continue, the buildup of scar tissue can eventually stop liver function. The liver is located in the upper right side of the abdomen below the ribs. It has many essential body functions. These include:
- producing bile, which helps your body absorb dietary fats, cholesterol, and vitamins A, D, E, and K
- storing sugar and vitamins for later use by the body
- purifying blood by removing toxins such as alcohol and bacteria from your system
- creating blood clotting proteins
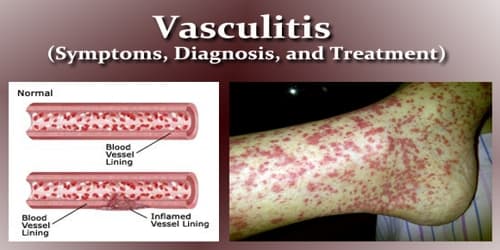
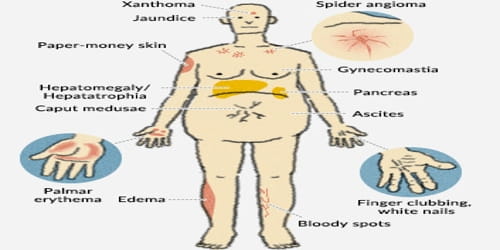
Typically, the disease develops slowly over months or years. Early on, there are often no symptoms. As the disease worsens, a person may become tired, weak, and itchy, have swelling in the lower legs, develop yellow skin, bruise easily, have fluid buildup in the abdomen, or develop spider-like blood vessels on the skin.
For cirrhosis to develop, long-term, continuous damage to the liver needs to occur. When healthy liver tissue is destroyed and replaced by scar tissue, the condition becomes serious, because it can start blocking the flow of blood through the liver.
Cirrhosis is most commonly caused by alcohol, hepatitis B, hepatitis C, and non-alcoholic fatty liver disease. A number of less common causes of cirrhosis include autoimmune hepatitis, primary biliary cholangitis, hemochromatosis, certain medications, and gallstones. Diagnosis is based on blood testing, medical imaging, and liver biopsy.
Cirrhosis is serious because of the importance of the organ it affects. The liver, weighing about three pounds and roughly the size of a football, is the largest of the body’s internal organs. Among its many functions, the liver serves as an essential part of the digestive system by producing bile, which is stored in the gallbladder, then released into the small intestine, where it helps break down fatty food. The liver also helps maintain the proper composition of the blood by regulating the amounts of fat, protein, and sugar that enter the bloodstream.
Causes, Sign, and Symptom of Cirrhosis: Cirrhosis occurs as the result of long-term injury to the liver. Possible causes include viruses, genetic deficiencies, prolonged obstruction of bile flow, and long periods of exposure to drugs and other toxic substances. In the majority of cases, however, the culprit is excessive consumption of alcohol.
The most common causes of cirrhosis are long-term viral hepatitis C infection and chronic alcohol abuse. Obesity is also a cause of cirrhosis, although it is not as prevalent as alcoholism or hepatitis C. Obesity can be a risk factor by itself, or in combination with alcoholism and hepatitis C.
People with cirrhosis may have few or no symptoms and signs of liver disease. Some of the symptoms may be nonspecific and don’t suggest the liver is their cause. Common symptoms and signs of cirrhosis include:
- Yellowing of the skin (jaundice) due to the accumulation of bilirubin in the blood
- Fatigue
- Weakness
- Loss of appetite
- Itching
- Easy bruising from decreased production of blood clotting factors by the diseased liver.
People with cirrhosis of the liver also develop symptoms and signs from the complications of the disease.
Diagnosis and Treatment of Cirrhosis: The gold standard for diagnosis of cirrhosis is a liver biopsy, through a percutaneous, transjugular, laparoscopic, or fine-needle approach. The best predictors of cirrhosis are ascites, platelet count <160,000/mm3, spider angiomata, and a Bonacini cirrhosis discriminant score greater than 7.
Additional tests that can evaluate the liver include:
- upper endoscopy (to see if esophageal varices are present)
- ultrasound scan of the liver
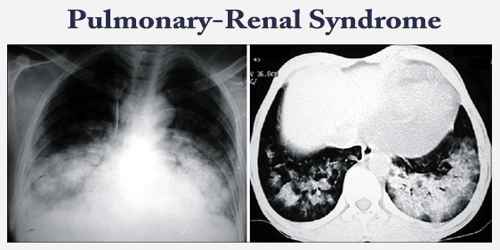
- MRI of the abdomen
- CT scan of the abdomen
- liver biopsy (the definitive test for cirrhosis)
If the cirrhosis is diagnosed early enough, damage can be minimized by treating the underlying cause or the various complications that arise.
- Medications: The patient may be prescribed drugs to control liver cell damage caused by hepatitis B or C.
- Controlling pressure in the portal vein: Blood can “back up” in the portal vein that supplies the liver with blood, causing high blood pressure in the portal vein. Drugs are usually prescribed to control the increasing pressure in other blood vessels. The aim is to prevent severe bleeding. Signs of bleeding can be detected via an endoscopy.
- Banding: A small band is placed around the base of the varices to control bleeding.
- Injection sclerotherapy: After an endoscopy, a substance is injected into the varices, which triggers a blood clot and scar tissue to form. This helps stem the bleeding.
- Transplantation: If complications cannot be controlled or when the liver ceases functioning, liver transplantation is necessary. Survival from liver transplantation has been improving over the 1990s, and the five-year survival rate is now around 80%. The survival rate depends largely on the severity of the disease and other medical risk factors in the recipient.
- A Sengstaken-Blakemore tube with a balloon: A balloon is placed at the end of the tube. If endoscopy does not stop the bleeding, the tube goes down the patient’s throat and into their stomach. The balloon is inflated. This places pressure on the varices and stops the bleeding.
- Infections: The patient will be given antibiotics for any infections that arise.
- Screening for liver cancer: Patients with cirrhosis have a much higher risk of developing liver cancer. The doctor may recommend regular blood tests and imaging scans.
- Palliative care: Palliative care is specialized medical care that focuses on providing patients with relief from the symptoms, pain, and stress of a serious illness, such as cirrhosis. The goal of palliative care is to improve quality of life for both the patient and the patient’s family and it is appropriate at any stage and for any type of cirrhosis.
- Treatment for alcohol dependency: It is important for the patient to stop drinking if their cirrhosis was caused by long-term, regular heavy alcohol consumption. In many cases, the doctor will recommend a treatment program for treating alcohol dependency.
In some cases, the damage caused by cirrhosis covers most of the liver and cannot be reversed. In these cases, the person may need a new, transplanted liver. It can take time to find a suitable donor, and this procedure is often advised only as a last resort.
Information Source: