Bipolar disorder, formerly known as manic depression, is a mood disorder marked by periods of depression followed by periods of abnormally elevated happiness that last from days to weeks. You may feel sad or hopeless when you are depressed, and you may lose interest or pleasure in most activities. If the elevated mood is severe or associated with psychosis, it is referred to as mania; if it is milder, it is referred to as hypomania. When your mood shifts to mania or hypomania (a milder form of mania), you may feel euphoric, energized, or unusually irritable. Sleep, energy, activity, judgment, behavior, and the ability to think clearly can all be affected by mood swings.
Mania causes an individual to act or feel abnormally energetic, happy, or irritable, and they frequently make rash decisions with little regard for the consequences. During manic phases, there is usually a reduced need for sleep. During depressive episodes, the individual may cry, have a negative outlook on life, and make poor eye contact with others. Suicide is a significant risk; over a 20-year period, 6% of those with bipolar disorder committed suicide, while 30-40% engaged in self-harm. Bipolar disorder is frequently associated with other mental health issues, such as anxiety disorders and substance use disorders.
While the exact causes of bipolar disorder are unknown, genetic and environmental factors are thought to play a role. Many genes, each with minor effects, may play a role in the disorder’s development. About 70-90% of the risk of developing bipolar disorder is due to genetic factors. A history of childhood abuse and long-term stress are two environmental risk factors.
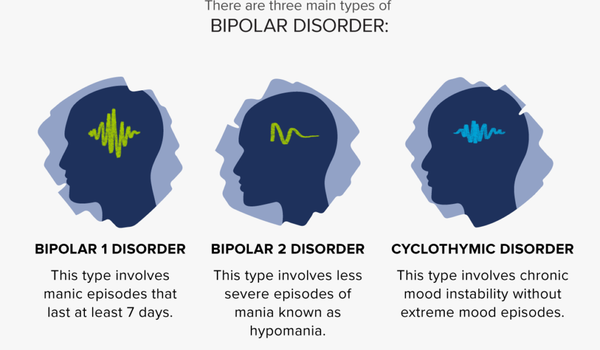
If there has been at least one manic episode, with or without depressive episodes, the condition is classified as bipolar I disorder, and as bipolar II disorder if there has been at least one hypomanic episode (but no full manic episodes) and one major depressive episode. These symptoms are not diagnosed as bipolar disorder if they are caused by drugs or medical problems. Attention deficit hyperactivity disorder, personality disorders, schizophrenia, and substance use disorder, among many other medical conditions, have symptoms that overlap with bipolar disorder. A diagnosis does not require medical testing, though blood tests or medical imaging can rule out other issues.
Despite the mood swings, people with bipolar disorder frequently fail to recognize how much their emotional instability disrupts their lives and the lives of their loved ones, and as a result, they do not receive the necessary treatment. And, if you’re like some people with bipolar disorder, you might enjoy the euphoria and productive cycles. This euphoria, however, is always followed by an emotional crash that can leave you depressed, exhausted, and possibly in financial, legal, or relationship trouble.
The mainstay of long-term pharmacologic relapse prevention is lithium and certain anticonvulsants such as valproate and carbamazepine, as well as atypical antipsychotics such as aripiprazole. Antipsychotics are also used during acute manic episodes and when mood stabilizers are either poorly tolerated or ineffective. Long-acting injectable formulations are available for patients who are concerned about compliance. There is some evidence that psychotherapy can help with the progression of this disorder.
The use of antidepressants in depressive episodes is debatable: they can be effective but have been linked to the onset of manic episodes. As a result, treating depressive episodes is frequently difficult. Electroconvulsive therapy (ECT) is effective in treating acute manic and depressive episodes, particularly those accompanied by psychosis or catatonia. If a person poses a risk to themselves or others, they may be admitted to a psychiatric hospital; involuntary treatment may be required if the affected person refuses treatment.