Lower social cohesion was linked to an antibody response to the COVID-19 vaccine, according to a new study by researchers from the Universities of Limerick and Stirling in the UK that was just published in the journal Brain, Behavior, and Immunity. People who experience less social cohesion also feel more isolated, which contributed to the decline in antibody responses to the vaccine.
This study is a famous example of mind-body medicine, which holds that our emotions, which are produced as a result of social interaction, can affect our immune systems.
Why is this important?
Our adaptive immune system’s capacity to combat diseases like COVID-19 depends heavily on antibodies. In order to tackle the virus globally, COVID-19 vaccines were used, as we have learned during the current epidemic. It was crucial to get the vaccine because the antibodies that were created after immunization provided defense against hospitalization and death.
However, following this and other vaccinations, persons who do not produce enough antibodies are frequently susceptible to infection or re-infection, which is why obtaining booster doses is also advised.
Stress, immunity, and the pandemic
It is generally known that elements like stress have an impact on human immunity, including the antibody response to vaccination. According to research, long-term stress has a detrimental effect on our immune system, making us more susceptible to infections, causing more inflammation and other disorders, and impairing our ability to produce antibodies in response to immunizations.
In contrast, research has also found that better quality social relationships and higher social support have been found to boost immunity (e.g., low levels of inflammation) and increase antibody levels following vaccination.
As a result, these psychosocial factors stimulate the areas of our brains where we think about and process information related to them, which in turn sets off a biological chain reaction that affects our capacity to produce antibodies.
We looked to see if the same kinds of social stressors experienced during the pandemic would also have a negative impact on the COVID-19 antibody responses because of the detrimental effects that stress has on people’s immune systems, particularly its damaging effect on antibody responses to vaccinations.
As we have all observed, stress was pervasive during the COVID-19 pandemic, with issues of misinformation and public trust coming to the fore, as well as managing multiple lockdowns, job losses, increased social restrictions, and lower social engagement all contributing to increased social stress. We focused on social cohesion as a key predictor of antibody responses.
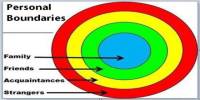
The idea of social cohesion encompasses our relationships, sense of belonging, and willingness to help and communicate with others as well as our level of trust in our neighbors. For example, during the initial lockdowns in Europe a sense of “being in it together” was an oft-used mantra to increase social cohesion and public adherence to public measures, as this was seen as a way of working together to fight the virus.
In fact, this was evident from the “clap for carers” in the UK, Italians singing from balconies, and Dubliners playing bingo in the flats, all of which increased social cohesion and public trust.
The author (Stephen Gallagher) noted that these feelings of social cohesion and trust, though fleeting, were caused by what UK researchers now refer to as the “Dominic Cummings effect,” in which the political elite violated and disregarded public health recommendations, which sparked outrage from the general public, which was thought to be largely compliant with these measures.
In the US, declining levels of trust were also observed throughout these times as levels of skepticism in science and governments reemerged, negatively affecting the adherence to public health recommendations. Lockdowns were also linked to less social interaction and a higher risk of loneliness. Given their importance, it made reasonable to investigate if social cohesiveness and loneliness had an impact on the responsiveness of the COVID-19 antibody.
How did we conduct this research?
We used data from over 600 people who took part in the UK’s Understanding Society COVID-19 antibody study in March 2021.
Participants were sent out a blood sampling kit and asked to provide a blood sample. They had to affirm whether they had received the COVID-19 vaccination, how many doses they had received it, whether they were infected, and whether they were lonely in addition to answering questions about their opinions about social cohesiveness and infection.
The survey results on social cohesiveness and loneliness were combined with the antibody titer studies performed on the blood samples in a lab.
What did we find?
We found that those participants who reported lower levels of social cohesion had a poorer antibody response to the COVID-19 vaccine. For instance, fewer antibodies were produced by people who felt less a part of their community and had less faith in their neighbors than by people who reported higher levels of these feelings. Additionally, those who reported lower social cohesion also frequently reported feeling more alone, which in turn decreased their immune response.
What does this all mean?
Given that the pandemic is still present and that vaccination is a key approach for combating COVID-19, this study shows that non-immune system-related characteristics like trust, connections, and loneliness are also crucial for it.
Additionally, social cohesiveness and loneliness are adjustable and can be used to enhance the reactivity of vaccines. Additionally, these findings emphasize once more how important social cohesiveness and public trust are to the effectiveness of our pandemic response.