Vitamin D is an important nutrient that helps to maintain overall health, including brain function. While vitamin D is known to help with bone health and calcium absorption, new research suggests that it may also help with neuronal development and function, including the brain’s dopamine circuit. Using cutting-edge technology, neuroscientists at The University of Queensland have discovered how vitamin D deficiency affects developing neurons in schizophrenia.
Professor Darryl Eyles has built on previous research from his Queensland Brain Institute laboratory linking maternal vitamin D deficiency and brain development disorders such as schizophrenia to better understand the functional changes occurring in the brain.
Schizophrenia is linked to a variety of developmental risk factors, both genetic and environmental. While the precise neurological causes of the disorder are unknown, it is known that schizophrenia is associated with a significant change in the way the brain uses dopamine, the neurotransmitter known as the brain’s “reward molecule.”
What we found was the altered differentiation process in the presence of vitamin D not only makes the cells grow differently, but recruits machinery to release dopamine differently.
Professor Eyles
Professor Eyles investigated the mechanisms underlying abnormal dopamine release and discovered that maternal vitamin D deficiency affects the early development and later differentiation of dopaminergic neurons.
The Queensland Brain Institute developed dopamine-like cells to mimic the process of differentiation into early dopaminergic neurons that occurs during embryonic development. They cultured the neurons both with and without the active vitamin D hormone. Dopamine neurite outgrowth was significantly increased in three different model systems. They then discovered changes in the distribution of presynaptic proteins involved in dopamine release within these neurites.
“What we found was the altered differentiation process in the presence of vitamin D not only makes the cells grow differently, but recruits machinery to release dopamine differently,” Professor Eyles said.
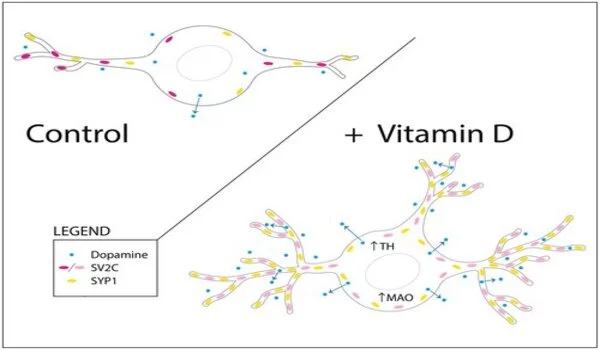
Using a new visualisation tool known as false fluorescent neurotransmitters, the team could then analyse the functional changes in presynaptic dopamine uptake and release in the presence and absence of vitamin D. They showed that dopamine release was enhanced in cells grown in the presence of the hormone compared to a control.
“This is conclusive evidence that vitamin D affects the structural differentiation of dopaminergic neurons.”
Dopamine is a neurotransmitter that plays a variety of roles, including reward and motivation, movement control, mood regulation, and cognitive processes. Dopamine system disruptions have been linked to a variety of neurological and psychiatric disorders, including Parkinson’s disease, schizophrenia, and addiction.
Professor Eyles and his colleagues were able to expand on their long-held belief that maternal vitamin D deficiency affects the formation of early dopaminergic circuits by leveraging advances in targeting and visualizing single molecules within presynaptic nerve terminals.
The researchers are now investigating whether other environmental risk factors for schizophrenia, such as maternal hypoxia or infection, alter the trajectory of dopamine neuron differentiation in the same way. Eyles and his colleagues believe that such early changes in dopamine neuron differentiation and function may be the neurodevelopmental basis of later dopamine dysfunction in adults with schizophrenia.