Burns have always been a tragedy for man. It has significant morbidity and, often, significant mortality. The incidence in the developing world burns are an even more important problem with over 2 million burns a year thought to occur in India and subcontinent. Mortality in the developing world is also much higher. Females, very young and the very old of both sexes are more vulnerable group to burn injuries. Throughout the country, an estimated 1% of the population suffers from different types of burns each year. Severity of burns injury depends on the degree of the burns and the area of the body affected . Burns may be superficial, involving just the epidermal layer of the skin, Partial-thickness burns involve the entirety of the epidermis and a portion of the dermis, full thickness, involving all layers of the skin and deeper structures. The extent of the injury is expressed in percentage of total body surface area (TBSA) involved.
For many years, partial-thickness burns have been treated by washing and cleaning of the wound, followed by a topical application of antimicrobial agent. For the control of infection, detailed bacteriological monitoring is recommended. The main therapeutic fields for prevention of infection are: immunotherapy, antisepsis, aseptic techniques, and rapid restoration of the destroyed body surface. The most important part of antisepsis in burns is topical treatment. Topical antiseptics like silver sulphadiazine, silver nitrate, bacitracin, povidone iodine, chlorhexidine, mupirocine are the most common substances used world -wide in burn care facilities.
For many decades, since 1968, silver sulphadiazine (SSD) has been used to treat burns and chronic wounds to overcome the problem of wound infection because of topical silver
Sulphadiazine cream has a broad spectrum of antimicrobial activity, is soothing, low development of bacterial resistance, few adverse reactions and a low risk of systemic toxicity. Silver sulfadiazine does not penetrate eschar so it is ineffective against already established burn wound infections. It requires frequent application and occasionally reported local skin reactions, such as pain, burning, or itching and hypersensitivity. A transient leukopenia secondary to bone marrow suppression often occurs with use of silver sulfadiazine in large burns. It may leave black tattoos from silver ion and mild inhibition of epithelialization may occur. Silver sulphadiazine with an excellent spectrum of activity, low toxicity, minimal pain is still the most frequently used topical agent for burn dressing
Povidone-iodine (PVP-I) is a effective disinfectant which can be used successfully in the treatment of bums and wounds. As an iodophor, povidone-iodine slowly liberates iodine when in contact with the skin or mucous membranes. It is active against both Gram-negative and Gram-positive bacteria, including Slaphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli and Klebsiella species. Povidone-iodine also possesses very marked antimycotic activity and is one of the few preparations really effective against Candida albicans. It is easy to apply, causes the patient minimal discomfort and be easy to remove for visualization of the wound. The ointment would result in a soft, more pliable type of crust which would allow easier movement by the patient without the tendency to crack over the flexor surfaces. In case of deep burn dressing with povidone iodine the possible disadvantage is the systemic iodine resorption with resulting thyroid and renal dysfunction. The high serum and urine iodine levels returned rapidly to normal after discontinuing the application and no disorders of thyroid function were revealed, and the TRH test indicated no abnormal reactions of the hypothalamus-pituitary axis.
Surgical Anatomy & Physiology of the Skin
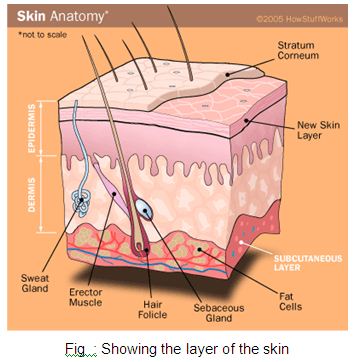
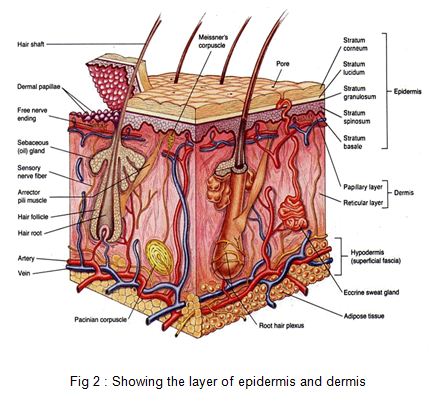
The skin is the largest organ of the body, ranging in area from 0.25 m2 in the newborn to 1.8 m2 in the adult. It consists of two layers: the epidermis and the dermis (corium) .The outermost cells of the epidermis are dead cornified cells that act as a tough protective barrier against the environment, including bacterial invasion and chemical exposure. The inner cells of the epidermis are metabolically active, producing compounds like growth factor, which help the ongoing replication process every two weeks. The epidermis contains five layers from bottom to top the layers are named: stratum basale ,stratum spinosum ,stratum granulosum ,stratum licidum stratum corneum. There are three types of specialized cells in the epidermis-
i) the melanocyte produces pigment (melanin)
ii)the Langerhans’ cell is the frontline defense of the immune system in the skin
iii) he Merkel’s cell’s function is not clearly known
Much progress has been made in the management of patients with burns, especially in the treatment of shock and systemic complication but topical antimicrobial agents have not been very extensively studied. Topical antimicrobial therapy is the single most important component of the wound healing in hospitalized burn patients. Infection caused by the proliferation of pathogenic organisms, chiefly bacteria and fungi, is the foremost problem in treatment. It is important, therefore, to search for locally applicable preparations capable of effectively disinfecting the surface of the burnt area. The principal requirements of such a preparation are that it is non-irritant, painless, easily applied (i.e. spreads well), less expensive, good eschar penetration and is without effect on acid-base balance.
A significant difference was observed between povidone-iodine and silver sulphadiazine in healing times and decrease in the number of positive bacterial cultures.
The aim of this clinical trial is to evaluate the effectiveness of Povidone Iodine in comparism with silver sulphadiazine in partial-thickness burns with regard to wound infection, length of hospital stay, number of dressings, rate of eschar formation and doses of analgesics used. So this study will help to identify an ideal topical antimicrobial agent for partial thickness burn dressing.
The second, thicker layer, the dermis (0.06–0.12 mm), is composed chiefly of fibrous connective tissue. The dermis contains the blood vessels and nerves to the skin and the epithelial appendages of specialized function like sweat glands. The nerve endings that mediate pain are found in the dermis. The dermis is a barrier that prevents loss of body fluids by evaporation and loss of excess body heat. Sweat glands help maintain body temperature by controlling the amount of water that evaporates. The dermis is also interlaced with sensory nerve endings that mediate the sensations of touch, pressure, pain, heat, and cold. This is a protective mechanism that allows an individual to adapt to changes in the physical environment. The two layers of the dermis are the papillary and reticular layers. The upper, papillary layer, contains a thin arrangement of collagen fibers. The lower, reticular layer, is thicker and made of thick collagen fibers that are arranged parallel to the surface of the skin. The skin produces vitamin D, which is synthesized by the action of sunlight on certain intradermal cholesterol compounds.
Pathology & Pathophysiology of Thermal Injuries
Burn causes coagulative necrosis of the epidermis and underlying tissues, with the depth depending on the temperature to which the skin is exposed and the duration of exposure. The specific heat of the causative agent also affects the depth.
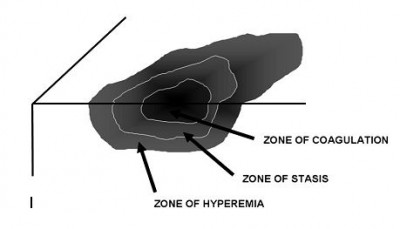
The microscopic pathologic feature of the burn wound is principally surface coagulation necrosis. Jackson’s 1947 state that burned tissue has three distinct zones. The first is the zone of “coagulation,” or necrosis with irreversible cell death and no capillary blood flow. Surrounding this is a zone of injury or stasis, characterized by sluggish capillary blood flow and injured cells. Although damaged, the tissue is still viable. Further tissue
Fig. 3 : Zones of injury. Thermal energy can be visualized as producing three concentric spheres of injury. The innermost is the zone of coagulation, the middle sphere is the zone of stasis, and the outermost is the zone of hyperemia.
injury can be caused by products of inflammation such as oxidants and vasconstrictor mediators. Environmental insults such as hypoperfusion, desiccation, or infection can also cause the injured tissue to become necrotic. This process is called wound conversion. The third zone is that of “hyperemia,” which is the usual inflammatory response of healthy tissue to nonlethal injury. Vasodilatation and increased capillary permeability is typically present.
A rapid loss of intravascular fluid and protein occurs through the heat-injured capillaries. The volume loss is greatest in the first 6–8 hours, with capillary integrity returning toward normal by 36–48 hours. A systemic inflammatory response occurs in response to a large body burn, resulting in the release of oxidants and other inflammatory mediators into unburned tissues. This leads to a shift of extracellular sodium and water into the intracellular space. Smoke inhalation markedly increases the hemodynamic instability, fluid requirements, and mortality rates by adding another source of intense inflammation leading to local lung and systemic tissue damage.
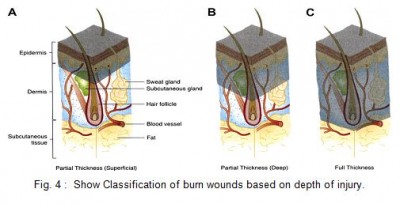
Traditionally, burns have been classified as first-, second-, and third-degree, but the current emphasis on burn healing has led to classification as partial-thickness burns, which can heal spontaneously, and full-thickness burns, which require skin grafting, although deep partial-thickness burns are usually excised and grafted as well.
A first-degree burn involves only the epidermis and is characterized by erythema and minor microscopic changes; tissue damage is minimal, protective functions of the skin are intact, skin edema is minimal, and systemic effects are rare. Pain, the chief symptom, usually resolves in 48–72 hours, and healing takes place uneventfully. In 5–10 days, the damaged epithelium peels off in small scales, leaving no residual scarring. The most common causes of first-degree burns are overexposure to sunlight and brief scalding.
Second-degree or partial-thickness burns are deeper, involving all of the epidermis and some of the corium or dermis. The systemic severity of the burn and the quality of subsequent healing are directly related to the amount of undamaged dermis. Superficial burns are often characterized by blister formation, while deeper partial-thickness burns have a reddish appearance or a layer of whitish, nonviable dermis firmly adherent to the remaining viable tissue. Complications from superficial second-degree burns are mainly severe pain related. These burns usually heal with minimal scarring in 10–14 days unless they become infected. Deep dermal burns heal over a period of 4–8 weeks .Conversion to a full-thickness burn by bacteria is common. Skin grafting of deep dermal burns, when feasible, improves the biologic quality and appearance of the skin cover.
Full-thickness (third-degree) burns have a characteristic white, dry, waxy appearance and may appear to the untrained eye as unburned skin. Burns caused by prolonged exposure to heat, with involvement of fat and underlying tissue, may be brown, dark red, or black. The diagnostic findings of full-thickness burns are lack of sensation in the burned skin, lack of capillary refill, and a leathery texture that is unlike normal skin. All dermal epithelial elements are destroyed, leaving no potential for reepithelialization.
Topical agents and Burn wound care
Timely and effective use of antimicrobials has revolutionized burn care by decreasing invasive wound infections. An untreated burn wound rapidly becomes colonized with bacteria and fungi because of the loss of normal skin barrier mechanisms. Each wound is dressed with an appropriate covering that serves several functions. First, it protects the damaged epithelium, minimizes bacterial and fungal colonization, and provides splinting action to maintain the desired position of function. Second, the dressing is occlusive to reduce evaporative heat loss and minimize cold stress. Third, the dressing needs to provide comfort over the painful wound.
Topical agents have definitely advanced the care of burn patients. Topical antiseptics like silver sulfadiazine, silver nitrate, bacitracin, povidone iodine, chlorhexidine, mupirocine are the most common substances used world -wide in burn care facilities.
Silver sulfadiazine is the most commonly used. It has a broad spectrum of activity because its silver and sulfa moieties cover gram-positive, most gram-negative, and some fungal forms. Some Pseudomonas species possess plasmid-mediated resistance. Silver sulfadiazine is relatively painless on application, has high patient acceptance, and is easy to use. Occasionally, patients complain of a burning sensation after it is applied, and in a few patients, a transient leukopenia develops 3 to 5 days after its continued use. This leukopenia is generally harmless and resolves with or without cessation of treatment.
PVP-I, which is iodine complexed with polyvinyl pyrolidone, is a widely used and highly potent antiseptic that eradicates all classes of pathogens responsible for nosocomial infections, including Gram-positive and Gram-negative bacteria, as well as antibiotic-resistant strains and spores (bacterial and fungal), viruses, mycobacteria, and protozoa. As iodine liberated from the PVP molecule, it exerts its antimicrobial effect in less than a minute, with most organisms being destroyed in 15 to 30 seconds or less; the mechanisms involved in these effects include an irreversible combination of iodine with tyrosine residues of proteins, interference with the formation of hydrogen bonding by some amino acids and nucleic acids, oxidization of sulphydryl groups, and reaction with sites of unsaturation in lipids. All these advantages make PVP-I a good candidate for the topical treatment of burns.
Severe complications are rare. Extended long term treatment and repeated irrigation of wounds and cavities can provoke abnormal thyroid gland function, hepatic or renal insufficiencies, metabolic acidosis, convulsions, neutrogena, etc.
| A Chart show summary of the antibacterial activity of the some drugs. | ||||||||
| Staphylococcus | Pseudomonas | Proteus | E. coli | Streptococci | Clostridium | Candida | Virus | |
| Silver sulphadiazine | +++ | +++ | +++ | ++ | + | ++ | +++ | |
| Mafenide | + | +++ | ++ | ++ | +++ | + | + | |
| Silver nitrate | +++ | ++ | N | |||||
| Nitrofurazone | ++ | + | +++ | ++ | +++ | +++ | N | N |
| Chlorhexidine | +++ | ++ | ++ | +++ | + | +++ | ||
| Povidone iodine | +++ | +++ | +++ | +++ | +++ | +++ | +++ | +++ |
| +++ = excellent activity; ++ = active; + some activity N = no activity | ||||||||
Aims and Objectives
General objectives:
The aim of this clinical trial was to evaluate the effectiveness of povidone iodine in comparison with that of silver sulfadiazine for partial-thickness burn dressing.
Specific objectives:
- to compare the efficacy of povidone–iodine with that of silver sulphadiazine for preventing burn wound infections.
- Comparative evaluation of effectiveness of povidone iodine and silver sulfadiazine regarding : number of burn dressing , rate of eschar formation , length of hospital stay, doses of analgesics used.
Ultimate objectives :
To identify an ideal topical antimicrobial agent for burn dressing with an broad spectrum of antimicrobial activities, less toxic , easy to apply and having no effect on wound healing.
Materials and methods
Study design : A Prospective study.
Place of study : Departments of surgery,
Sher-E-Bangla Medical College Hospital, Barisal.
Study period : August, 2008 to December,2010
Study model : Patients with partial thickness of burn admitted
in the Department of surgery. Sher-E-Bangla
Medical College Hospital, Barisal.
Sample size : 50 cases Partial –thickness of burn caused by
scalding or flames.
Sampling technique: Simple random sampling, lottery method.
Selection criteria:
Inclusion criteria:
These patients with partial-thickness of burn who entered the study had a burn area of 10–40% of total body surface area (TBSA) age > 12yrs caused by scalding or flames.
Exclusion criteria:
Patients who had 3rd degree burns (contact burn and others), contaminated wounds (with chemical or faecal material, or soil), co-morbid diseases, inhalation injury, fractures, neurological injury or who were pregnant and age <12years were excluded from the study. Patient who has reported any allergic reaction to povidone iodine or silver sulfadiazine also excluded from the study.
Study Procedure:
The sample size will be divided in two groups :
Group A(n=25): The first group is the controlled group (i.e. the SSD group) was treated by washing and cleaning with normal saline, followed by topical application of 1% silver sulfadiazine dressing.
Group B(n=25): The second group is the study group (i.e. the PVP-I group) was treated by washing and cleaning with normal saline, followed by topical application of 5% povidone iodine ointment dressing.
The study population included patients of both sexes (male or female) with partial thickness burn admitted to the different units of surgery department of Sher-E-Bangla Medical College Hospital, Barisal from August, 2008 to December, 2010.
Study protocol is approved by the institutional ethical committee of Sher-E- Bangla Medical College, Barisal. The nature of the study was fully explained to each patient and written informed consent was obtained before they were enrollment in the study.
On admission all patients had a full medical history recorded. A complete physical examination was undertaken. The extent, site of the burn and whether superficial or deep was recorded. The cause of the burn was also established. Partial thickness burn defined as superficial partial thickness involved enter epidermis and part of dermis characterized by formation of blister. 50 patients with partial thickness burn were randomized for closed dressing with either 5% PVP-I ointment and 1% SSD cream ( 25 patients in each group). When necessary, analgesics were given and intravenous fluids administered.
During application of the medication to burn wound a record was kept of: (I) the degree of pain experienced (mild, moderate or severe); (ii) the ease of spread of the preparations (excellent, satisfactory or poor); and (iii) the removal of the dressing (easy or difficult).(iv) the number of dressing needed. The respective topical agent was reapplied until the wound had healed. If needed normal saline was used for surgical wash. If antibiotics were required during the study this was recorded. The decision to give antibiotics was based on bacterial culture and sensitivity. Dressing was changed regularly when it was shocked and patient complain discomfort.
Pain recorded according to visual analog pain scale contains a range of numbers starting at 0 and going up to 10. The higher the number, the more intense the pain. On this scale, a 0 indicates that the patient feels no pain. The numbers from 1 to 3 indicate a mild level of pain, numbers from 4 to 7 reflect a moderate degree of pain, numbers from 7 to 10 are reserved for severe pain of an amount that is disabling in nature. The patients compliance about the local antimicrobial agent was recorded during dressing of the burn wound.
The following were checked daily: (i) the patient’s mental state (ii) general condition of the patient, including hydration, temperature; (iii) the degree of wound healing – the wound edge was inspected for evidence of wound infection (secretion of pus) cellulitis, healing was defined as complete epithelialization of the burnt area, and the rate of wound healing was recorded; and (iv) evidence of systemic infection, e.g. septicaemia or abscess formation at distal sites; any other medical complications were also recorded.
Bacterial swabs were taken from the burn surface, 1st at the 5 – 7th day then weekly and the cultured organisms identified and antibiotic was advised accordingly.
Patients of both group discharged after complete wound healing and advice for take a follow up after 30 days.
All Data collected by data collection form and they are distributed in a tabulated form for analysis. Quantitative data is analyzed by rate, ratio, proportion and percentage and qualitative data based on works by mean and standard deviation. Significant differences were evaluated using the unpaired Student’s t test and Chi-square test with the help of MS Xcel-07 and SPSS-17. P- Value <0.05 differences were considered as significant level for statistical comparisons.
Ethical measure :
This study protocol was approved by institutional ethical committee of SBMCH, Barisal. All patients were given an explanation of the study and informed consent was taken. The study was not involved any expensive investigative procedures and significant risk, as well as economic burden to the patient.
Result
The study population included patients of both sexes (male or female) of different age group with partial thickness burn admitted to the different units of surgery department of Sher-E-Bangla Medical College Hospital, during the study period.
50 patients with partial thickness burn were randomized for closed dressing with either 5% povidone iodine ointment and 1% silver sulphadiazine ( 25 patients in each group).
The observation is recorded in data collection sheet and distributed in the table for analyze. Quantitative data was analyzed by rate, ratio, proportion and percentage and qualitative data based on works by mean and standard deviation. Significant differences were evaluated using the unpaired Student’s t test and Chi-square test.
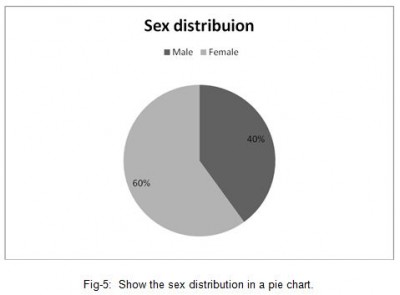
| Table I : Sex distribution of the patients ( n=50 ) | ||||||||
| Sex | Group | Total/percent | ||||||
SSD
Group(n-25 ) PVP-I Group(n=25) Male91120(40%) Female161430(60%)
In this study, SSD group comprises of 9 male and 16 female and in the PVP-I group, 11 male and 14 female patients. This table revels that the incidence of burn was more in female than in the male. Total number of male was 20(40%) and female was 30 (60%).
Total number of male was 20(40%) and female was 30 (60%).The sex ratio in the study male: female was 2:3.
| Table-II : Age distribution of the burn patient ( n=50) | ||
| Age of the patient in years | Number of the patient | |
| SSD group (n=25) | PVP-I group (n=25) | |
| 15-25 | 8(16%) | 9(18%) |
| 25-35 | 11(22%) | 8(16%) |
| 35-45 | 4(8%) | 6(12%) |
| 45-55 | 2(4%) | 2(4%) |
| Total | ||
| Mean age in years | 30±4.08 | 30.4±4.00 |
Age distribution of the burn patient (n=50), the age range between 16yrs to 52 randomly divided in two groups, the table-II, show that 17 (34%) patients within the 15-25 yrs of age, 19 (38%) within 25-35 years. The mean age in SSD group was 30± 4.08 and the mean age of PVP-I group was 30.4± 4.00 (mean age of the study population was 30.2±4.04). So there was no age difference had been observed in the sample between the study and the controlled group.
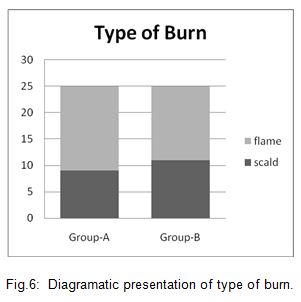
| Table III : Distribution of burn type (n=50 ) |
| Burn type Number of cases Total/ percentage |
| SSD PVP-I |
Scaled 9 11 20 (40%)
Flame 16 14 30 (60%)
In this study 30(60%) patient came with flamed burn and 20 (40%) with scald burn. Maximum number of patient of group A and the group-B came with flame burn
Both group contain maximum number of patients with flamed burn and hrere was no sinficant difference has been observed between two group in the type of burn.
| Table IV : Time Distribution of hospital arrival ( n=50 ) | |||
| Duration between burn and hospital arrival in hour | Number of patient | ||
| Group-A | |||
(SSD Group) Group-B
(PVP-I Group) <6126-12111012-1810918-2424>2410
In case of burn injury heeling rate is highly depend on early starting of the wound management. In this study the most of the patients (Group-A, 21 and group-B, 19) came within 6 – 18 hrs, only 3 patients came before 6 hrs and 1 patient came after 24hrs. The mean time of hospital arrival in SSD group is 12.8hrs and PVP-I group 12.6hrs.
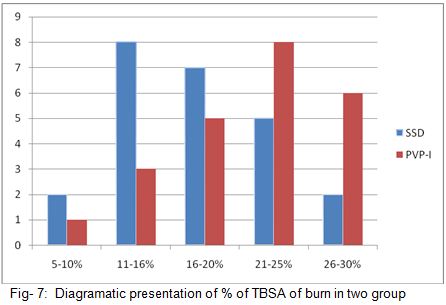
| Table V : % TBSA of burn distribution (n=50) | |||||
| % of Bur | |||||
Number of cases SSD Group=25 PVP-I
Group=25 5-10 2 1 11-15 8 3 16-20 7 5 21-25 5 8 26-30 2 6 31-35 1 2 Mean % TBSA 17.5±3.06 21.7±2.2
* Data are given as means ± SD,
The percent TBSA area of burn range from 5 to 35% in both groups. Mean % TBSA of burn in SSD Group 17.5±3.06 and in PVP-I 21.7±2.2. So percentage TBSA of burn is more in study group.
Diagram representing the % TBSA of burn between two study group shown that in case of burn area of 5-20% the number of case was more in SSD Group, but in case of 21-30% burn the number was more in PVP-I group. Most of the patient came with 11-25% burn in both study group. The SSD-group had the highest number of cases in 11-16 % burn, on the other hand the PVP-I group had the highest number in 21-25%.burn.
| Table VI : Pain intensity distribution (n=50) | |||
| Pain intensity in | |||
Visual analog scaleNumber of patient Group-A
(SSD Group)
n=25(%) Group-B
(PVP-I Group)
n=25(%) Mild(1-3)7(28)10(40)Moderate(4-6)10(40)9(36)Sever (7-9)8(32)6(24)Mean Pain intensity5.12±0.754.52±0.77
Data are given as means ± SD
In SSD group among 25 patient, 17(68%) patients complained mild to moderate and 10(40%) patients expressed sever pain experience, in the PVP-I group, 19(76%) patients reported mild to moderate and 6(24%) complained sever pain experience. The mean pain intensity in case of SSD-group was 5.12±0.75 and in the PVP-I group was 4.52±0.77. In chi- quire test the value 2.66 is less than the table value (p=0.05) and is not significant.
| Table-VII : Distribution of patient compliance during application and removal of the topical antimicrobial agents(n=50) |
During application- Preparations
Spread SSD Group
n (%)PVP-I Group
n(%)
Excellent
7(28)
16(64)Satisfactory12(48)7(28)Poor6(24)2(8)
Removal of the preparationSSD Group
n(%)PVP-I Group
n(%)
Easy and painless
6(24)
20(80)Difficult and pain full19(76)5(20)
Table VII : Represent during application of the topical agent regarding spreading over the burned area the responder compliance for SSD : 7(28%) excellent, 12(48%) satisfactory and 6(24%) poor, for PVP-I : 16(64%) reported excellent, 7(28%) satisfactorily and 2(8%) poor. The value of chi-squire test ( at df-2 ) 6.838 was more than the table value (p=0.05) difference. So the null hypothesis was rejected. Povidone iodine was well spread during application to the burn wound according to the responder compliance.
During removal of preparation easy and painless reported by 6(24%) cases in SSD group and 20(80%) cases in PVP-I group; Difficult and pain full reported by 19(76%) patient in case of SSD group and 5(20%) patient in PVP-I group.
Count :
| Removal of the local agent | Total | ||||
| Group of the patient | Easy and painless | Difficult and | |||
pain fullPearson
Chi-Squire test PVP-I2052515.705SSD61925 Total262450
proportions compared with the use of Pearson chi-squared test.
So the pearson chi-square test value 15.705, is more than the table value of (p=0.001) with the df-1, so the null hypothesis is rejected and value is highly significant. So PVP-I ointment was more easily and painlessly removable preparation according to responder compliance.
| Table-VIII : Wound observation both group (SSD=25,PVP-I=25) | ||||
| Number of cases in | ||||
1st weekNumber of cases in
2nd week ObservationSSDPVP-ISSDPVP-IN(%)N(%)N(%)N(%) Pus/Slough /necrosed tissue4(16)2(8)8(32)5(20)Pseuedo scar14(28)1(4)17(68)2(8)Bacterial swap smear positive8(32)2(8)8(32)4(16)New epithelialization4(16)6(24)15(6021(84)
The wound of the SSD group shows pus/slough or necrosed tissue in 4 (16%) patient in the 1st week and 8 (32%) at the end 2nd week; in the PVP-I group 2 ( 8%) patient at the 1st week and 5 ( 20%) patient at the end of the 2nd week developed the same.
Discussion
The extent and depth of burn wounds are established shortly after admission.
Severity of burns injury depends on the degree of the burns and the area of the body affected. Burns involve the entirely of the epidermis and a portion of the dermis estimate as a Partial-thickness burn. The extent of the injury is expressed in percentage of total body surface area (TBSA) involved. Once the extent and depth of the wounds have been assessed and the wounds have been thoroughly cleaned an debridement was done , the management phase begins. 50 patients with partial thickness burn were randomized for closed dressing with either 5% PVP-I ointment and 1% SSD cream (25 patients in each group). The group-A (SSD group) is the controlled group with the traditional use of 1% silver sulphadiazine, the group-B( PVP-I group) is the study group with the use of 5% povione iodine ointment for dressing of burn wound.
In the study Group-A (SSD group ) comprises 9(36%) male and 16(64%) female; in the Goup-B (PVP-I Group ), 11 (44%) male and 14(56%) female patient so total number of male is 20(40%) and female is 30 (60%). The table-I, revels that the incidence of burn is more in female than in the male. The sex ratio in the study male: female was 2:3.
Women wearing “Shari” or” Orna” are the major victims for the flame burn-this occurs mainly in the home during household work like cooking, particularly from gas leakage or burst stoves, and setting clothes alight. Epidemiology of burn study report suggest that two-thirds of burns occur in the home, of which 60% are associated with cooking. So the sex ratio in this study is supported by previous study.
Age distribution of the burn patient (n=50), the age range between 16yrs to 52 randomly divided in to groups, the table-II, show that 36 (72%) patient within the 15-25 yrs of age, 14( 28%) within 35-55 years. The mean age of the study population 30.2±4.04 yrs.
Though very younger and the very older group is susceptible to burn injury they are out of the study due exclusion criteria because of their high mortality and morbidity. Epidemiological study of burn reveals that Overall, 20% of all burns occur in children up to the age of 4, 10% of burns occur between the ages of 5 and 14, 60% of burns occur between the ages of 15 and 64, of which half are flame burns.
The mean age in SSD group is 30± 4.08 yrs and the mean age of PVP-I group is 30.4±4.00yrs. So there is no significant age difference between two group.
The table III, represent 30(60%) patient came with flamed burn and 20(40%) with scald burn. Maximum number of patients are flamed burn in both study and controlled group, Threre is no sinficant difference between two group in the type of burn. Other study report “Burn and Plastic Surgery Unit in Bangladesh, September 2007 suggest that percentage of flamed burn is about 75% in our country. The majority of burns in children are scalds caused by accidents with kettles, pans, hot drinks and bath water. Among adolescent patients, the burns are usually caused by young males experimenting with matches and flammable liquids. In adults, scalds are not uncommon but are less frequent than flame burns.
In case of burn injury healing rate is highly depend on early starting of the wound management. The table IV the most of the patients ( Group-A 21 and group-B 19) came within 6 – 18 hrs, within 6 hrs came only 3 patient, after 24hrs 1 patient. The mean time of hospital arrival in SSD group was 12.8hrs and PVP-I group was 12.6hrs. So there is no significant difference is observed in hospital arrival and delay of starting of treatment between the control group-A and the study group-B.
Varying degrees ( 5-35%) burn percentage is estimated during admission according to the rule of nines and most of the patient admitted with 11-25% TBSA burn in both group. The extensive burned patient are not include in the study criteria. The variable placed in table-V, show that , The SSD group posses highest number of cases with 11-16 % burn on the other hand the PVP-I group posses the highest number with 21-25%, the mean % of TBSA of burn in SSD group was 17.5±3.06 and in PVP-I group was 21.7±2.2. So in the group-B, the patients have comparatively lager % TBSA of burn.
Pain experience of the patient at the end of 1st week according to visual analog pain scale contains a range of numbers starting at 0 and going up to 10. The higher the number, the more intense the pain. On this scale, a 0 indicates that the patient feels no pain. The numbers from 1 to 3 indicate a mild level of pain, such an annoying or nagging amount experienced from an ache or a minor injury. The numbers from 4 to 7 reflect a moderate degree of pain, to the extent that it interferes with the patient’s everyday activities. The numbers from 7 to 10 are reserved for severe pain of an amount that is disabling in nature. A 10 is the highest imaginable amount of pain.
In the table-V, Pain intensity distribution show that in the SSD group among 25 patients, 18( 72%) shown mild to moderate and 10( 40%) shown sever pain experience ; in the PVP-I group 19 ( 76%) patients reported mild to moderate and 6 (24%) complained sever pain experience. The mean pain intensity in case of SSD group counted 5.12±0.75 and in the PVP-I group counted 4.52±0.77. In chi- quire test the value 2.66 is less than the table value (p=0.05), is not significant. So the conclusion is that PVP-I do not reduces significant amount of pain in burn dressing. Another comparative study on Hydrogel dressing versus SSD dressing conducted in Gujrat, India from June 2005 –November 2006 on 50 cases documented that in the Hydrogel dressing group, 72 % of patients showed a pain score up to 2( mild) while patient dressing with conventional SSD, 76 % of patients showed a pain score up to 6 (moderate). A study conducted by Ahmed Nurus Sami et al, at IMMC, Rowalpindi, Pakistan during Jan. 2007 – Jun. 2009 on 50 burn patients“ Honey Compared with Silver Sulphaiazine as Burn Wound Dressing documented that burn patients dressing with honey were rendered pain free early, mean pain was relieved by 12th day, while dressing with SSD mean pain was relieved by 16.8 days.
Table VII : Represent the responder compliance during application of the topical agent regarding spreading over the burned area for SSD : 7(28%) patients reported excellent, 12(48%) reported satisfactory and 6(24%) poor ; for PVP-I: 16(64%) reported excellent , 7(28%) satisfactorily and 2(8%) poor. The value of chi-squire test ( at df-2 ) 6.838 is more than the table value (p=0.05 ). So null hypothesis is rejected. Povidone iodine is well spread during application to the burn wound according to the responder compliance. A study named “A new povidone-iodine cream for the treatment of burns Comparison with a standard topical regimen”, supported that the povidone iodine cream has an excellent spreading properly over the wound than other conventional agents.
During removal of preparation easy and painless reported by 6(24%) cases in SSD group and 20(80%) Cases in PVP-I group and difficult and pain full reported by 19(76%) patient in case of SSD group and 5(20%) patient in PVP-I group. The pearson chi-square test value 15.705 , is more than the table value of (p=0.001) with the df-1, so the null hypothesis is rejected and test result is highly significant. So PVP-I ointment is more easily and painlessly removable preparation according to responder compliance. Previous study supported that Povidone iodine is more better than the conventional topical regiment for their easy application and removing during dressing and 98% acceptance to the responer.
In the the table- VIII: The wound of the SSD group shows pus or slough in 4 (16%) patient in the 1st week and 8 (32%) at the end 2nd week, in the PVP-I group 2 ( 8%) patient at the 1st week and 5 ( 20%) patient at the end of the 2nd week developed the same. The table- VIII also show that 8 (32%) patients shows bacterial smear positive in SSD group and 2 (8% ) shows in PVP-I group at the 1st week at the 2nd weeks the SSD group shown 8 (32%) and PVP-I shown 4 (16%) bacterial positive smear.
Rate of infection is more in the controlled group-A ( SSD group) than the study group so it is speculated that the povidone iodine reduces the rate of infection and decrease pus formation in comparison to SSD. As silver sulfadiazine does not penetrate eschar, it is ineffective against already established burn wound infections. As an iodophor, povidone-iodine slowly liberates iodine when in contact with the skin or mucous membranes. It is active against both Gram-negative and Gram-positive bacteria, including Slaphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli and Klebsiella species. Povidone-iodine also possesses very marked antimycotic activity.
It is also supported by an another study in Baquba General Hospital, Diyala, Iraq, over a period of three months, in 2006 “How to Decrease the Incidence of Eschar Formation During the Use of Topical Povidone- Iodine Ointment in the Treatment of Burns” shown that povidone iodine reduces the number of bacterial count 23% per day and count reduces to 0% within 4-5 days after application.
Formation of pseudo scar in 14 ( 56%) cases at the 1st week and in 17 ( 68%) cases at the 2nd week in SSD group and in the PVP-I group, 1 ( 4%) patient at 1st week and 2 ( 8%) at the 2nd week . It is noteworthy that the formation of pseudo eschar is about 50-60% more in SSD group. Other study report reveals that the incidence of eschar formation was 100% in silver sulphadiazine in which PVP-I ointment was used topically during the full course of treatment; this percentage fell to 2.3. The study also suggested, in an attempt to prevent eschar formation, PVP-I can be used for the first 4 days post-injury followed by SSD, with excellent results .The formation of eschars after use of PVP-I in burn patients can be easily treated with the application of 10% salicylic acid without any complications and avoiding surgical escharotomy.
In SSD group 4 (16%) patient developed new epithelialization within 1st week and 15 (60%) patient at the end of 2nd week on the other hand in PVP-I group 6 ( 24 %) patient in the 1st week and 21 (84%) at the end of 2nd week developed the same. So the rate of epethelialization is slightly higher in the study group.
Some study shows that there is no significant change in healing time between silver sulphadiazine and povidone iodine. There is considerable controversy concerning the effect of PVP-I on wound healing with regard to both in vitro and in vivo studies. While Kietzman and Vogt et al. reported an improvement in the healing process when using PVP-I, Niedner found that PVP-I did not prolong the total wound healing time. In contrast, Kramer reported in his review that in most instances PVP-I did not effectively promote good wound healing and that most studies showed impaired wound healing. It has been found that low concentrations of PVP-I are toxic to keratinocytes, fibroblasts, and collagenolytic enzymes: these cells and enzymes are most prevalent in the proliferative and maturation phases of wound healing.
The table IX represent the total number dressing of the burn patient were needed during their hospital stay. The mean number of dressing in SSD group 19±2.40 and in the PVP-I group is 14.9±2.90. Several studies on burn dressing with SSD have shown that more number of dressing is essential for partial thickness burn wound than need in the PVP-I.
The decrease in rate of infection and early healing reduced the total number of dressing in Group –B (PVP-I group). A study on burn patient “ Xenoerm versus 1% SSD in Partial Thickness Burn” in 2009, on 76 patients shown that patient dressing with SSD needed 10.9±9.1 number of dressing and mean hospital stay 11.5±15.5.
The data represent in the table –X represent that the most of the patient, 16 (64%) in SSD group, 22 (88%) in PVP-I group take discharge in the end of the second week. The mean hospital stay in the SSD group is 12.32±3.64 and in the PVP-I the mean hospital stay is 10.40±3.63. In the student’s (unpaired) ‘t’ test value 2.22 is more than the table value (p=0.05), so null hypothesis is rejected . In the group B with PVP-I dressing reduces the significant number of hospital stay. Others study reports have shown that burn patient dressing with SSD needed 13-21 days hospital stay. This short hospital stay was due to faster reepithelialisation, reduction of wound infection and fewer wound dressing changes.
All patient advised for follow up after 30 days from the date of discharge only 32 patient responded, among them, 18 from the Group-A (SSD Group), 12 patient from the Group-B
( PVP-I group). The table XI show that in the group-A, among 18 patient,15 cases were scar free and scar developed 3 cases. On the other hand in group-B among 12 , 11 cases were scar free 1 patient developed scar. Ratio of scar formation among the follow up patients, in the SSD group is 6: 1 whereas in the PVP-I group 12: 1. So the rate of scar formation was two times more in the SSD group of patients.
Conclusion and recommendation
It is important to search for locally applicable preparations capable of effectively disinfecting the surface of the burnt area. The principal requirements of such a preparation are that it is non-irritant, painless, easily applied (i.e. spreads well), less expensive, good eschar penetration and is without effect on acid-base balance.Silver sulphadiazine with an excellent spectrum of activity, low toxicity, minimal pain is still the most frequently used topical agent for burn dressing. The use of silver sulphadiazine is frequently associate with the development of pseudo-eschar, which can lead to error in the evaluation of burn depth by the observer. It does not penetrate eschar, so it is less effective against already established burn wound infections. In this study significant difference between topical use of povidone iodine and silver sulphadiazine was observed during partial thickness burn dressing, the povidone iodine reduces the healing time, the degree of pain experience, rate of eschar formation, the number of dressing , wound infections and duration of hospital stay.
For burn dressing povidone iodine is thus a better option than conventional silver sulphadiazine however, more studies are required to form a conclusion.