Researchers from The Wistar Institute, an international biomedical research leader in cancer, immunology, infectious disease, and vaccine development, have published a new study that demonstrates how crucial characteristics on the surface of HIV-infected cells aid the disease’s evasion of the immune system.
It also demonstrates how these functions can be turned off. The discoveries, which were published in the journal PLOS Pathogens, are the first step toward a new class of medication that aims to target cells carrying a persistent virus that prevents us from curing HIV infection.
“We identified a glyco-immune checkpoint interaction as a novel mechanism that allows HIV-infected cells to evade immune surveillance,” said Mohamed Abdel-Mohsen, Ph.D., assistant professor in the Vaccine & Immunotherapy Center at The Wistar Institute and co-author on the paper. “And we developed a novel approach that selectively targets these interactions on the surface of these infected cells.”
The holy grail of HIV research remains a cure or long-term remission. HIV can be reduced to undetectable levels with current medications, but it cannot be eradicated completely. When treatment is stopped, the condition usually returns soon.
HIV raises the chance of various health problems, such as neurological diseases, cardiovascular disease, and cancer, even when it is under control.
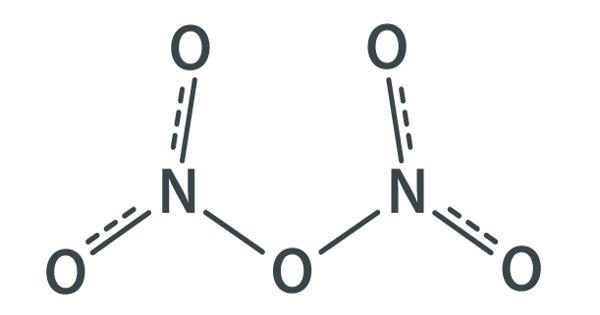
Researchers looked examined a sort of sugar molecule called sialic acid on the surface of HIV-infected cells for the new study. These sugars connect to siglecs, which are particular receptors on the surface of disease-fighting immune cells known as “natural killers.” When these receptors are activated, they operate as inhibitors, preventing killer cells from killing.
“We thought, is it possible that these HIV-infected cells are using this interaction covering themselves with these sugars to evade the natural killer immune surveillance?” said Abdel-Mohsen.
The Abdel-Mohsen team discovered that this was the case, and infected cells can use this inhibitory link to elude immune surveillance. Researchers next looked into manipulating this link in order to improve the killer cells’ ability to kill HIV-infected cells.
We identified a glyco-immune checkpoint interaction as a novel mechanism that allows HIV-infected cells to evade immune surveillance. And we developed a novel approach that selectively targets these interactions on the surface of these infected cells.
Mohamed Abdel-Mohsen
They first investigated if removing the inhibitors from the killer cells would allow them to unleash their full killing potential. Immune cells, on the other hand, may assault indiscriminately, eliminating both good and harmful cells.
After that, the researchers focused on the HIV cells. They utilized a sialidase enzyme to eliminate the sialic acid sugars that were causing the immunological inhibitors to activate. However, this damaged all cells once more, causing the killer cells to attack randomly.
Finally, a sialidase conjugate coupled to HIV antibodies was produced. Only sialic acid on HIV cells was targeted by this antibody-sialidase combination. The killer immune cells attacked and killed the HIV-infected cells after the sialic acid was removed from these cells, leaving healthy cells alone.
“The killer cells become a super killer for the HIV-infected cells and they now attack them in a selective manner,” said Abdel-Mohsen. “The discovery could be a missing link in the “shock and kill” approach to HIV treatment that has been a focus of research for the past several years,” he added.
The HIV is “shocked” out of latency so it can be discovered, and then the immune system is stimulated to “destroy” the virus once and for all in this two-step process.
While efficient strategies for reversing latency have been developed, scientists have yet to uncover a mechanism to make HIV-infected cells more killable once reactivated.
“We may have the shock, but we don’t have yet the kill,” Abdel-Mohsen said. “Our method actually increases the susceptibility of HIV-infected cells to killing, which is one of the top unmet needs in the HIV field.”
The team’s technique could be tried in tandem with widely neutralizing antibody therapy now being explored in clinical trials, according to first author Samson Adeniji, Ph.D., a postdoctoral researcher at Wistar. “By combining approaches, we could turn these immune cells from a cop into a kind of Robocop,” he said.
The researchers also mentioned that, in addition to HIV, the method might be used to treat other infectious diseases that elude the immune system, such as hepatitis and COVID.
Following that, the scientists will do animal tests to test their findings in vivo. They’re also looking into whether additional sugar compounds on HIV play a role comparable to sialic acid.
“HIV-infected cells are likely evading immune surveillance through many potential glyco-immune checkpoints,” Abdel-Mohsen said. “We are investigating other mechanisms and how to break them.”