According to a large, eight-year study published in the journal Radiology, people who have a history of allergic-like reactions to iodinated contrast media, which is used in a variety of X-ray-based procedures such as CT and angiography, are susceptible to similar reactions from commonly used MRI contrast agents. In addition, the study discovered that premedication or switching to a different MRI contrast agent may minimize risk in patients who have previously experienced contrast agent responses.
Gadolinium-based contrast agents (GBCA) have long been utilized to improve MRI visibility of organs, tissues, and blood vessels and provide a more accurate representation of disease. Although GBCA are relatively safe, newer studies have documented a number of side effects, including allergic-like hypersensitivity reactions such as redness and flushing.
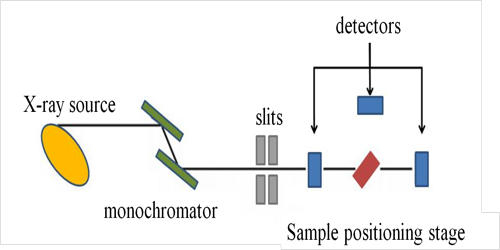
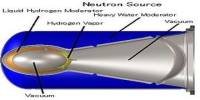
Gadolinium, like iodine, is a heavy metal that may absorb x-rays. Gadolinium has a greater atomic number (Z=64) than iodine (Z=53). Gadolinium’s k-edge is likewise more closely matched to the peak of the CT spectrum, implying that gadolinium absorbs a bigger fraction of the x-ray beam than iodine. However, because of the lower concentration and total number of gadolinium atoms used in modern formulations, gadolinium contrast is substantially less visible on CT than iodine contrast.
According to the study’s senior author, Hye-Ryun Kang, M.D., Ph.D., from the Department of Internal Medicine at Seoul National University College of Medicine in Seoul, Korea, the incidence of these reactions is increasing with the widespread use of GBCA, prompting an urgent need for research into risk factors.
Gadolinium-based contrast agents (GBCA) have long been utilized to improve MRI visibility of organs, tissues, and blood vessels and provide a more accurate representation of disease. As a result, clinicians should be aware that patients who have a history of hypersensitivity to one of the iodinated contrast media or GBCA are more likely to have hypersensitivity reactions to the other.
Hye-Ryun Kang
Dr. Kang and colleagues recently examined more than 330,000 cases of GBCA exposure in 154,539 patients at the Seoul National University Hospital over an eight-year period. There were 1,304 cases of allergic-like hypersensitivity reactions, representing a rate of 0.4%. The typical recurrence rate in patients who had previously experienced a GBCE reaction was 15%.
Acute allergic-like hypersensitivity reactions, or those that occur within one hour of contrast administration, accounted for 1,178 cases, while delayed allergic-like hypersensitivity reactions, or those that occur beyond the first hour and mostly within one week after exposure, accounted for 126 cases.
Those who had a history of allergic-like hypersensitivity reactions to iodinated contrast media were at a higher risk of allergic-like hypersensitivity reactions to GBCAs. Because of the structural and chemical distinctions between the two, a history of hypersensitivity to iodinated contrast media was traditionally not considered a risk factor for hypersensitivity to GBCAs and vice versa.
“The results of our study challenge this idea,” Dr. Kang said.

According to Dr. Kang, the increased risk could be due to a tendency to drug allergies in sensitive patients, rather than any cross-reactivity caused by structural similarities between iodinated contrast media and GBCA. In fact, those who had previously experienced a comparable reaction to GBCA were at a higher risk of hypersensitive reactions to iodinated contrast media.
“As a result, clinicians should be aware that patients who have a history of hypersensitivity to one of the iodinated contrast media or GBCA are more likely to have hypersensitivity reactions to the other,” she said.
Data analysis revealed that premedication with steroids and antihistamines, as well as altering the GBCA, had preventative effects in patients with a history of acute allergic-like hypersensitivity reactions. Patients who received premedication before MRI or were moved to a different GBCA had the lowest recurrence rate. Only premedication lowered the incidence of reactions in participants who had a history of delayed reactions.
“Because the most important preventive measure is to avoid the culprit agent,” Dr. Kang stated, “a precise record of previously used GBCA should be kept for all patients. Prior to MRI procedures, physicians should discuss proper premedication techniques with their patients.”
Dr. Kang underlined that contrast-enhanced MRI tests are invaluable in the diagnosis and monitoring of numerous disorders, and that the overall risk remains minimal. “Because the majority of these reactions are moderate,” she explained, “we believe the benefits of MRI outweigh the potential dangers associated with GBCA use.”
Dr. Kang recommends that all patients undergoing an MRI with GBCA exposure provide a full history of previous hypersensitive allergic reactions, and that relevant preventative measures, such as premedication and switching to various forms of GBCA, be adopted when necessary.
The researchers intend to undertake larger-scale investigations in the future to determine potential risk factors and effective prevention techniques for delayed hypersensitivity reactions to GBCA.