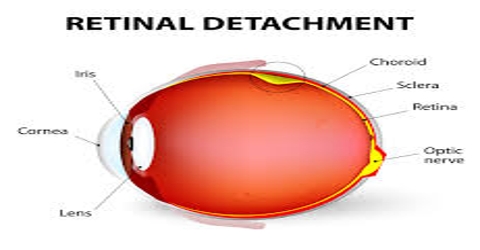
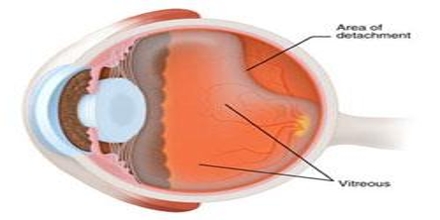
Retinal detachment happens when the retina becomes separated from the nerve tissues and blood supply underside it. A detached retina happens when the retina peels away, or detaches from its underlying layer of sustain tissue at the back of the eye. While painless, visually this has a clouding effect that has been likened to a grey curtain moving across the field of vision.
There are three types of detached retina:
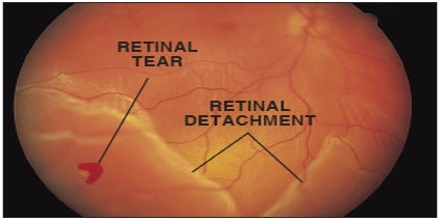
- Rhegmatogenous retinal detachment is a break, tear, or hole in the retina. This hole allows liquid to pass from the vitreous space into the subretinal space between the sensory retina and the retinal pigment epithelium.
- Secondary retinal detachment is also known as exudative retinal detachment or serous retinal detachment. It happens when inflammation, vascular abnormalities, or injury cause fluid to build up under the retina.
- Tractional retinal detachment is when an injury, inflammation, or neovascularization causes the fibrovascular tissue to pull the sensory retina from the retinal pigment epithelium.
Causes of Retinal Detachment
Retinal detachment happens when this layer is pulled from its usual position. Sometimes, there are little tears in the retina. These, too, can cause the retina to become detached.
The detached portion of the retina is no longer able to correctly transmit light signals to the brain. Vision can also be disrupted by retinal blood vessels that leak fluid into the internal segment of the eye where vitreous, or gel-like like fluid would usually be. If the retinal detachment progresses into the macula, or central part of the retina, the impact on vision can become more severe.
Symptoms of Retinal Detachment
An eye care expert can resolve retinal detachment through a number of retinal and pupil reaction tests, ranging from simple visual insight testing to an ultrasound of the eye.
For the patient, the grey curtain mentioned above occurs after retinal detachment has already begun. Before this happens, there are signs and symptoms that can alert one to the possible onset of retinal detachment, including:
- Eye floaters accompanied by eye flashes
- Sudden onset of blurred vision
- A sensation that a transparent curtain is coming down over the field of vision
- Shadows or blind spots in the field of vision
- Straight lines start to appear curved
Treatment for Retinal Detachment
If a doctor suspects retinal detachment, they will usually refer the patient to an eye expert, or ophthalmologist, for a precise diagnosis.
Surgery has proven a greatly successful treatment for retinal detachment, provided the situation has been detected early enough. To ensure that treatment can be effective, anyone experiencing the symptoms above should be given medical attention within 24 hours. Usual surgical measures include:
Laser surgery: Repairs tears in the retina that are the underlying cause of separation
Pneumatic retinoplexy: a tiny gas bubble is placed in the eye that floats the retina back into place; usually accompanied by laser surgery to ensure the retina stays in correct point everlastingly.
Scleral buckle: suturing a silicone “buckle” to the eye that indents the wall of the eye into a position that allows the retina to reattach.